Risk Adjustment Coder Resume Guide
Risk adjustment coders review and analyze patient medical records to assign codes that are used to determine the complexity of a patient’s condition. They must ensure accuracy in coding, while adhering to all applicable laws and regulations. Additionally, they provide feedback on coding issues and help create strategies for improving risk-adjustment processes.
Your expertise in risk adjustment coding is unmatched, and you’d make an invaluable addition to any medical facility. But hiring managers won’t know who you are unless you write a resume that stands out from the crowd.
This guide will walk you through the entire process of creating a top-notch resume. We first show you a complete example and then break down what each resume section should look like.
Table of Contents
The guide is divided into sections for your convenience. You can read it from beginning to end or use the table of contents below to jump to a specific part.
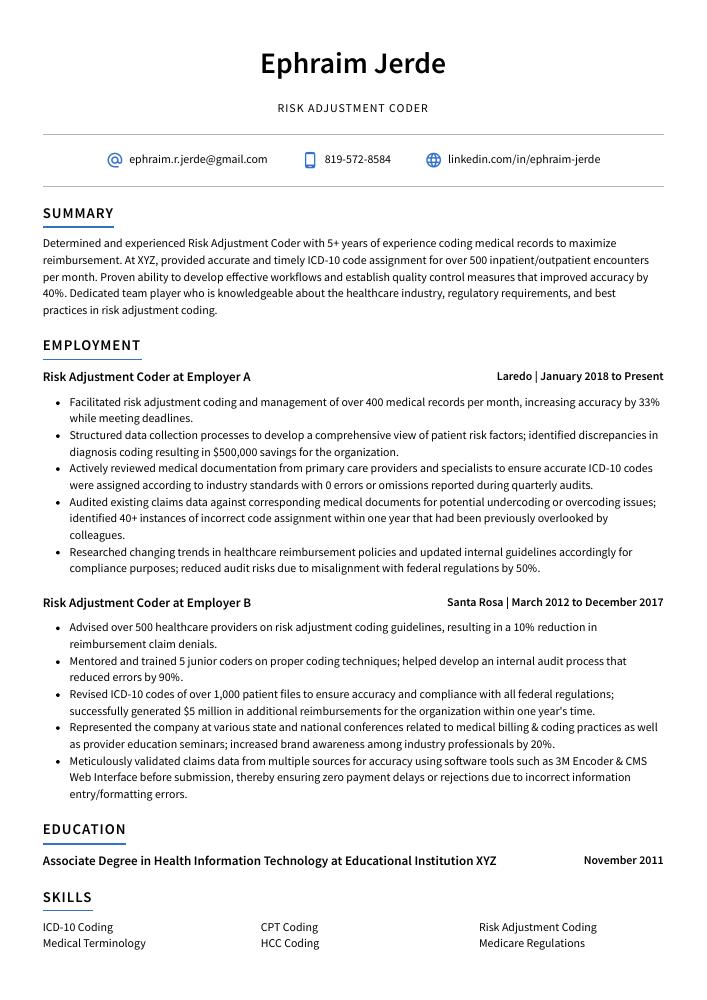
Risk Adjustment Coder Resume Sample
Ephraim Jerde
Risk Adjustment Coder
[email protected]
819-572-8584
linkedin.com/in/ephraim-jerde
Summary
Determined and experienced Risk Adjustment Coder with 5+ years of experience coding medical records to maximize reimbursement. At XYZ, provided accurate and timely ICD-10 code assignment for over 500 inpatient/outpatient encounters per month. Proven ability to develop effective workflows and establish quality control measures that improved accuracy by 40%. Dedicated team player who is knowledgeable about the healthcare industry, regulatory requirements, and best practices in risk adjustment coding.
Experience
Risk Adjustment Coder, Employer A
Laredo, Jan 2018 – Present
- Facilitated risk adjustment coding and management of over 400 medical records per month, increasing accuracy by 33% while meeting deadlines.
- Structured data collection processes to develop a comprehensive view of patient risk factors; identified discrepancies in diagnosis coding resulting in $500,000 savings for the organization.
- Actively reviewed medical documentation from primary care providers and specialists to ensure accurate ICD-10 codes were assigned according to industry standards with 0 errors or omissions reported during quarterly audits.
- Audited existing claims data against corresponding medical documents for potential undercoding or overcoding issues; identified 40+ instances of incorrect code assignment within one year that had been previously overlooked by colleagues.
- Researched changing trends in healthcare reimbursement policies and updated internal guidelines accordingly for compliance purposes; reduced audit risks due to misalignment with federal regulations by 50%.
Risk Adjustment Coder, Employer B
Santa Rosa, Mar 2012 – Dec 2017
- Advised over 500 healthcare providers on risk adjustment coding guidelines, resulting in a 10% reduction in reimbursement claim denials.
- Mentored and trained 5 junior coders on proper coding techniques; helped develop an internal audit process that reduced errors by 90%.
- Revised ICD-10 codes of over 1,000 patient files to ensure accuracy and compliance with all federal regulations; successfully generated $5 million in additional reimbursements for the organization within one year’s time.
- Represented the company at various state and national conferences related to medical billing & coding practices as well as provider education seminars; increased brand awareness among industry professionals by 20%.
- Meticulously validated claims data from multiple sources for accuracy using software tools such as 3M Encoder & CMS Web Interface before submission, thereby ensuring zero payment delays or rejections due to incorrect information entry/formatting errors.
Skills
- ICD-10 Coding
- CPT Coding
- Risk Adjustment Coding
- Medical Terminology
- HCC Coding
- Medicare Regulations
- HIPAA Compliance
- Quality Assurance
- Data Analysis
Education
Associate Degree in Health Information Technology
Educational Institution XYZ
Nov 2011
Certifications
Certified Professional Risk Adjustment Coder (CPC-RAC
May 2017
1. Summary / Objective
A resume summary/objective is the perfect place to showcase your qualifications as a risk adjustment coder. In this section, you can highlight your experience with ICD-10 coding and CPT codes, any certifications or special training you have received in the field of medical coding, and how many years of experience you have working with insurance companies. Additionally, it is important to mention any software programs that are familiar to you such as EncoderPro or 3M 360 Encompass.
Below are some resume summary examples:
Amicable Risk Adjustment Coder with 10+ years of experience in medical coding. Seeking to bring my wealth of knowledge and expertise to ABC Company, where I can apply the current coding standards while maintaining accuracy and compliance. At XYZ Corporation, completed over 7000 risk adjustment codes for Medicare Advantage (MA) members within two months, resulting in an 8% increase in reimbursements. Solid understanding of CPT-4/HCPCS guidelines as well as ICD-10 CM diagnostic codes.
Dependable and experienced risk adjustment coder with 5 years of experience coding for Medicare, Medicaid and commercial insurance plans. At XYZ Inc., worked on large-scale data sets to improve accuracy of codes used in payment systems. Expertise using CPT/HCPCS, ICD-10 CM/PCS and DRG code sets as well as E&M guidelines for correct reimbursement levels. Received recognition from colleagues for excellent work ethic and attention to detail when resolving complex coding issues.
Well-rounded risk adjustment coder with 8 years of experience in medical coding and billing processes. Skilled at accurately documenting diagnoses, procedures and treatment plans based on ICD-10 guidelines to ensure compliance with payer requirements. Seeking to join ABC Healthcare in a role that involves providing accurate risk assessment codes for patients’ records. Key achievements include reducing claim denials by 11% within 6 months.
Talented and dedicated Risk Adjustment Coder with 8+ years of experience in the healthcare industry. Proven ability to use ICD-10 and HCPCS coding principles to accurately code diagnoses, procedures, and services for various medical specialties. Experienced in conducting risk analysis and adjusting reimbursement rates according to government regulations. Strong organizational skills that ensure accuracy while meeting tight deadlines.
Proficient Risk Adjustment Coder with 5+ years of experience in medical coding and auditing. Seeking to join a team at XYZ where I can further develop my skillset and contribute to the success of a high-performing organization. Skilled in accurate risk adjustment coding for large groups, Medicare Advantage plans, Medicaid programs, PACE organizations, etc., as well as analyzing patient charts and records for correct diagnosis codes.
Hard-working risk adjustment coder with 7+ years of experience in coding and auditing medical records. Skilled in accurately assigning ICD-10 codes to ensure correct reimbursement for healthcare services. Proven record of success meeting deadlines, minimizing errors, and maintaining data accuracy according to industry standards. Seeking a position at ABC Medical Solutions to utilize my expertise in risk adjustment coding.
Energetic and detail-oriented Risk Adjustment Coder with 7+ years of experience in ICD-10 coding and Medicare Advantage claims processing. Seeking to join ABC Health Solutions to leverage knowledge of CMS guidelines, risk adjustment principles, and data validation procedures for a positive impact on patient care outcomes. At XYZ Company achieved 67% accuracy rate on complex medical records reviews within tight timelines.
Committed risk adjustment coder with 8+ years of experience in the healthcare field. Seeking a position at ABC Medical to utilize knowledge and expertise in ICD-10 coding, provider documentation review, and risk adjustment analysis. Proven success in identifying quality assurance issues while maintaining accuracy levels above 95%. Fully certified by AAPC since 2012.
2. Experience / Employment
For the experience section, you should list your employment history in reverse chronological order. This means that the most recent job is listed first.
When writing about what you did, use bullet points to make it easier for the reader to digest the information quickly. You want to provide detail and explain any quantifiable results achieved from your work.
For example, instead of saying “Coded medical records,” you could say, “Accurately coded over 500 medical records per month according to ICD-10 guidelines and CMS regulations; reduced coding errors by 20% through thorough review.”
To write effective bullet points, begin with a strong verb or adverb. Industry specific verbs to use are:
- Coded
- Audited
- Analyzed
- Documented
- Researched
- Interpreted
- Assessed
- Validated
- Reviewed
- Reconciled
- Processed
- Updated
- Corrected
- Reported
Other general verbs you can use are:
- Achieved
- Advised
- Compiled
- Coordinated
- Demonstrated
- Developed
- Expedited
- Facilitated
- Formulated
- Improved
- Introduced
- Mentored
- Optimized
- Participated
- Prepared
- Presented
- Reduced
- Reorganized
- Represented
- Revised
- Spearheaded
- Streamlined
- Structured
- Utilized
Below are some example bullet points:
- Coded over 10,000 diagnoses for inpatient and outpatient medical records using ICD-10 coding guidelines; achieved 95% accuracy rate.
- Assessed patient health risks by analyzing diagnostic codes, procedure codes and payment amounts on claims forms; identified $1 million worth of erroneous payments over a 3-year period.
- Resourcefully resolved discrepancies between diagnosis codes and billing information to ensure that all insurance claims were accurate and up-to-date before submission.
- Reviewed 500+ reports with detailed clinical descriptions to determine the most appropriate risk adjustment factor (RAF) score each month, resulting in cost savings of 15%.
- Reconciled RAF scores from previous years for 400+ patients in an effort to reduce potential audit issues; successfully reduced unapproved payments by 25%.
- Spearheaded risk adjustment coding activities for a team of 10 coders, ensuring compliance with federal regulations and overseeing the completion of over 1,500 patient charts per month.
- Participated in collaborative efforts to enhance operational efficiency; implemented new coding protocols that reduced rework by 28% and decreased turnaround times by 2 hours on average.
- Reduced total errors related to risk adjustment codes from 6% down to 0%, resulting in improved accuracy across all medical records submitted for claims processing.
- Substantially increased productivity through timely execution of various complex tasks such as reviewing clinical documentation & assigning appropriate ICD-10 codes; completed 95+ cases daily within specified deadlines without compromising quality standards or accuracy criteria set forth by CMS/AHIMA guidelines.
- Updated electronic health record (EHR) systems regularly with accurate data points captured during the chart review process, optimizing results & providing reliable outcomes regarding patient care & payment reconciliation.
- Formulated and documented medical record information to assign appropriate ICD-10 codes for over 400 risk adjustment claims, resulting in a 20% decrease in coding errors.
- Analyzed and validated patient data from providers’ electronic health records to ensure accuracy of all coded diagnoses; improved the overall quality score by 15%.
- Proficiently utilized CPT/HCPCS modifiers and E&M guidelines when assigning diagnosis codes according to accepted industry standards and practices.
- Reorganized existing databases of patients’ medical histories, claims information, lab results & prescription services with detailed attention to detail; reduced discrepancy rates by 30%.
- Interpreted physician orders accurately while optimizing reimbursement levels through the use of correct HCPCS Level II procedure code classifications; increased revenue collection rate by 10%.
- Presented and discussed risk adjustment coding audit results to medical directors, accurately identifying discrepancies and potential compliance issues; secured $400,000 in recoveries for the organization.
- Reported findings from Risk Adjustment audits on a timely basis with 95% accuracy rate; identified 10 previously overlooked errors during quarterly reviews of codes leading to additional savings of $50K+.
- Achieved 98%+ accuracy rate when reviewing documentation for assigned patient encounters and assigning appropriate ICD-10 codes; improved overall quality assurance ratings by 15%.
- Optimized process control procedures related to data collection activities across all departments by establishing best practices guidelines based on industry standards; reduced turnaround time per chart review by 50%.
- Efficiently managed workload while maintaining high level of consistency when auditing/reviewing over 300 charts daily against accepted HCC criteria set forth by Medicare Advantage programs.
- Streamlined risk adjustment coding procedures and improved accuracy by 15%, resulting in an increase of $1,000 in reimbursement payments.
- Developed protocols for capturing accurate risk-adjustment data from electronic medical records; validated over 1,200 codes across 400+ patient charts per week.
- Prepared detailed reports outlining the nature of ICD-10 diagnoses and associated complications to ensure compliance with all governing regulations while reducing errors by 10%.
- Confidently provided guidance on complex coding issues to clinical staff members and assisted in training new hire coders; reduced misidentification incidents by 20%.
- Spearheaded the implementation of a secure system that enabled remote access to confidential patient information using encrypted passwords and authentication measures for enhanced security purposes.
- Documented diagnostic and procedural codes for over 100 medical records daily, ensuring accuracy while adhering to ICD-10 coding guidelines; successfully decreased the rate of denied claims by 25%.
- Utilized a variety of software systems to review patient information and accurately identify risk adjustments; identified an average of 10+ additional diagnoses per month that had been previously overlooked.
- Independently performed quality assurance checks on coders’ data entry work, correcting errors in order to meet compliance standards set by insurance providers.
- Corrected any discrepancies between submitted documents and clinical documentation in electronic health record (EHR) system with 98% accuracy within 1 hour turnaround time frame or less when required.
- Expedited resolution process for complex cases with multiple comorbidities through comprehensive evaluation, leading to higher reimbursement rates for healthcare entities across 15 states nationwide.
- Introduced new coding protocols and auditing processes to improve accuracy of risk adjustment codes, resulting in a 24% decrease in errors.
- Improved efficiency within the department by streamlining documentation process and implementing automated systems; reduced coding time per patient record by 50%.
- Demonstrated expertise with ICD-10 CM/PCS code sets as well as HCC Risk Adjustment Model when assigning risk scores for over 1,500 patients every month.
- Reliably identified gaps or discrepancies between medical records and billing submissions to ensure compliance with CMS requirements across all levels of care.
- Compiled detailed reports on monthly claims data trends from various insurance providers, including Medicare Advantage Plans & Medicaid Managed Care Organizations (MCOs).
3. Skills
Two organizations that have advertised for a position with the same title may be searching for individuals whose skills are quite different. For instance, one may be looking for a coder with experience in ICD-10 coding and another may require knowledge of HCC codes.
It is therefore important to tailor the skills section of your resume to each job you are applying for, as this will help ensure that it passes through any applicant tracking systems used by employers.
In addition to listing relevant qualifications here, you can further discuss them in other areas such as the summary or experience sections.
Below is a list of common skills & terms:
- CPT Coding
- Data Analysis
- Documentation Accuracy
- HCC Coding
- HIPAA Compliance
- ICD-10 Coding
- Medical Terminology
- Medicare Regulations
- Quality Assurance
- Risk Adjustment Coding
4. Education
Adding an education section to your resume will depend on how far along you are in your career. If you just graduated and have no prior experience, include an education section below your objective statement. However, if you have years of coding experience to showcase, it might be better to omit the education section altogether.
If an education section is included, make sure to mention courses related to risk adjustment coding that demonstrate a good understanding of medical terminology and documentation guidelines for accuracy in claims processing.
Associate Degree in Health Information Technology
Educational Institution XYZ
Nov 2011
5. Certifications
Certifications are a great way to demonstrate your expertise in a particular field. They provide potential employers with evidence of your knowledge and skills, as well as show that you are committed to staying up-to-date on industry trends.
If the job posting mentions any certifications or qualifications that would be beneficial for the role, make sure to include them in this section of your resume. This will help give hiring managers an idea of how qualified you are for the position and set you apart from other applicants.
Certified Professional Risk Adjustment Coder (CPC-RAC
May 2017
6. Contact Info
Your name should be the first thing a reader sees when viewing your resume, so ensure its positioning is prominent. Your phone number should be written in the most commonly used format in your country/city/state, and your email address should be professional.
You can also choose to include a link to your LinkedIn profile, personal website, or other online platforms relevant to your industry.
Finally, name your resume file appropriately to help hiring managers; for Ephraim Jerde, this would be Ephraim-Jerde-resume.pdf or Ephraim-Jerde-resume.docx.
7. Cover Letter
A cover letter is a great way to introduce yourself and explain why you are the perfect candidate for the job. It is made up of 2-4 paragraphs that provide more detail than what’s in your resume.
Including an effective cover letter with your application can give you a competitive edge over other applicants as it allows recruiters to learn additional information about who you are and why they should hire you. Although not all jobs require one, writing a cover letter is highly recommended when applying for any role.
Below is an example cover letter:
Dear John,
I am interested in the Risk Adjustment Coder position at XYZ Company. With my experience as a certified coder and biller, I am confident that I would be a valuable asset to your team.
In my current role, I code and review patient medical records for risk adjustment purposes. I have experience with multiple coding systems, including ICD-9, CPT, and HCPCS. My thorough understanding of risk adjustment methodology has allowed me to successfully identify opportunities for improvement within the coding process.
In addition to my coding experience, I also have strong analytical skills. I often utilize data analytics to identify trends in coded data and make recommendations for process improvements. My ability to think critically has helped me contribute to increased accuracy and efficiency within the coding department.
I am eager to apply my skills and knowledge to help XYZ Company achieve its risk adjustment goals. Thank you for your time and consideration; I look forward to speaking with you soon about this opportunity.
Sincerely,
Ephraim
Risk Adjustment Coder Resume Templates
 Hoopoe
Hoopoe Indri
Indri Quokka
Quokka Bonobo
Bonobo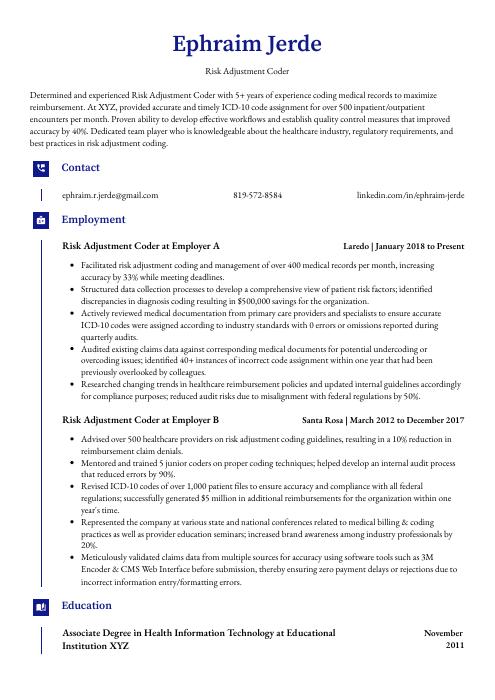 Gharial
Gharial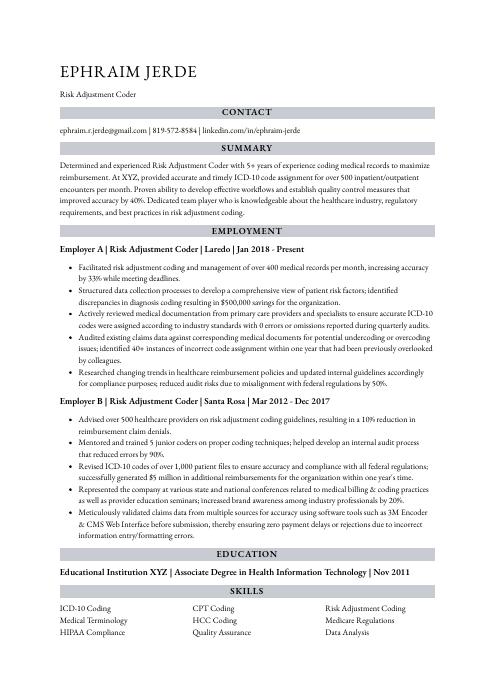 Numbat
Numbat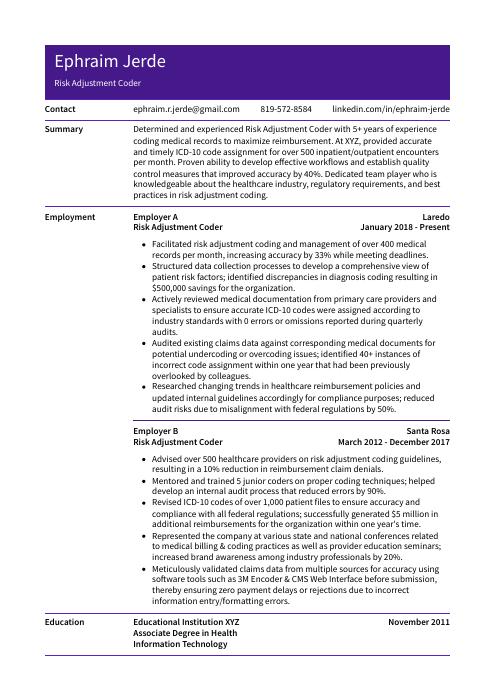 Pika
Pika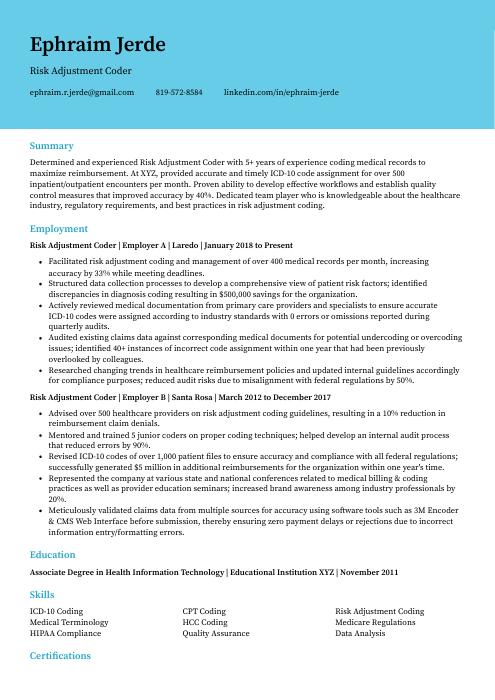 Dugong
Dugong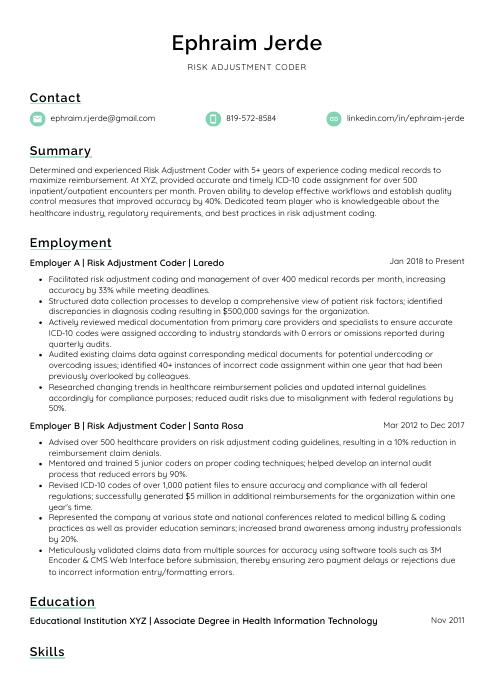 Lorikeet
Lorikeet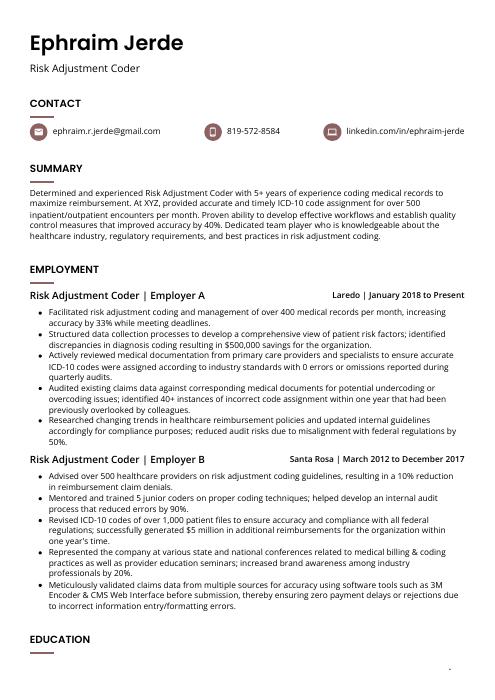 Fossa
Fossa Markhor
Markhor Echidna
Echidna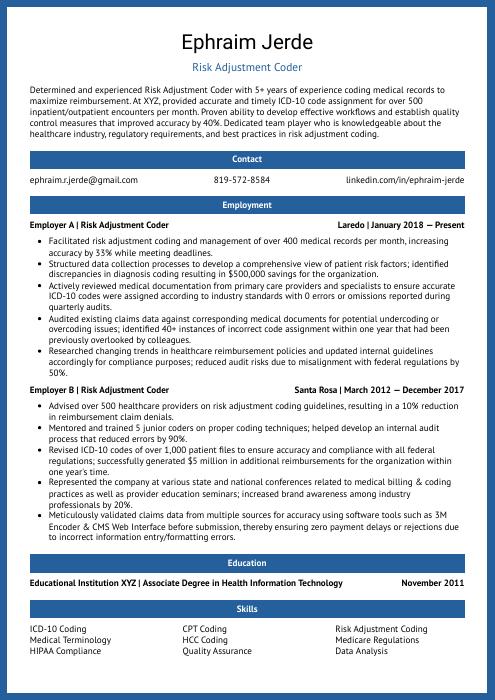 Ocelot
Ocelot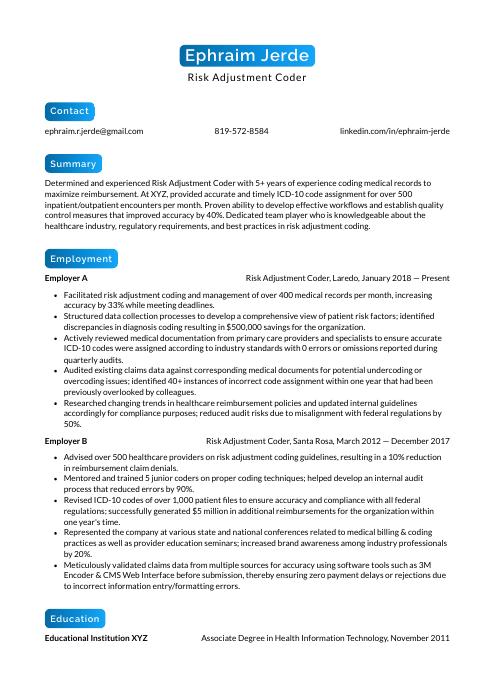 Kinkajou
Kinkajou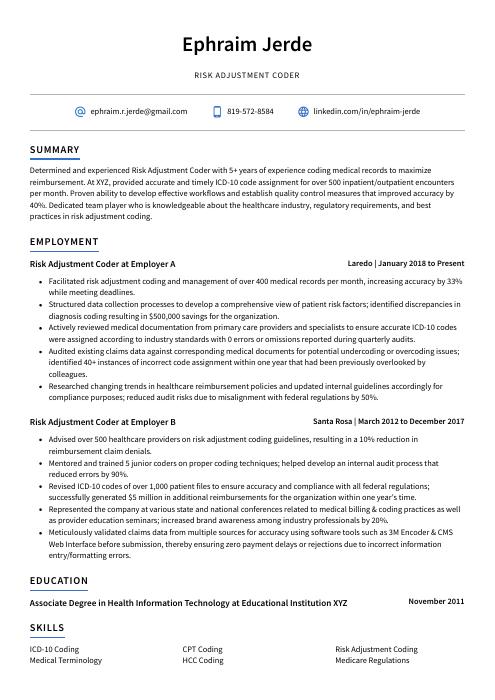 Axolotl
Axolotl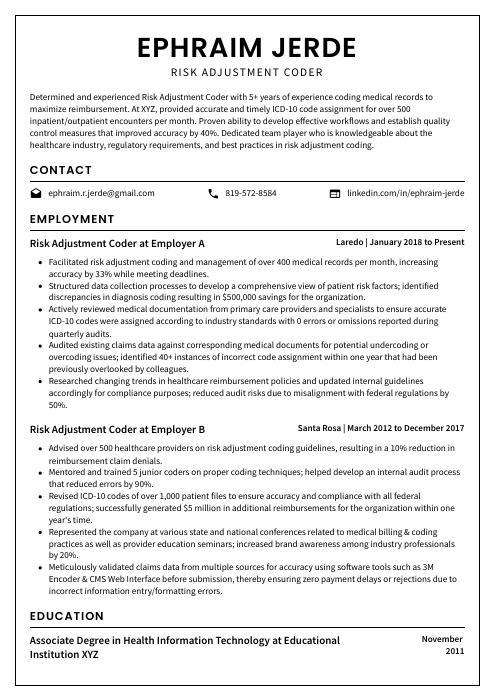 Cormorant
Cormorant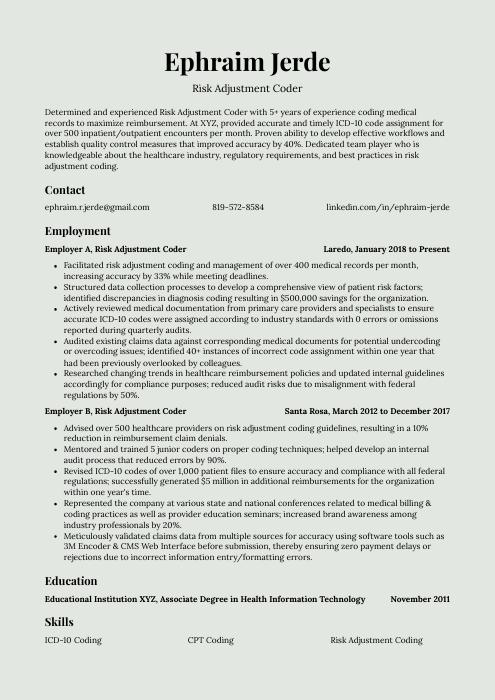 Saola
Saola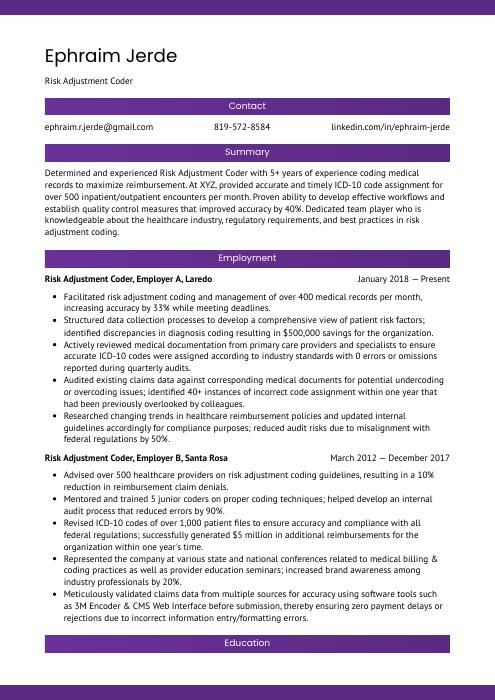 Jerboa
Jerboa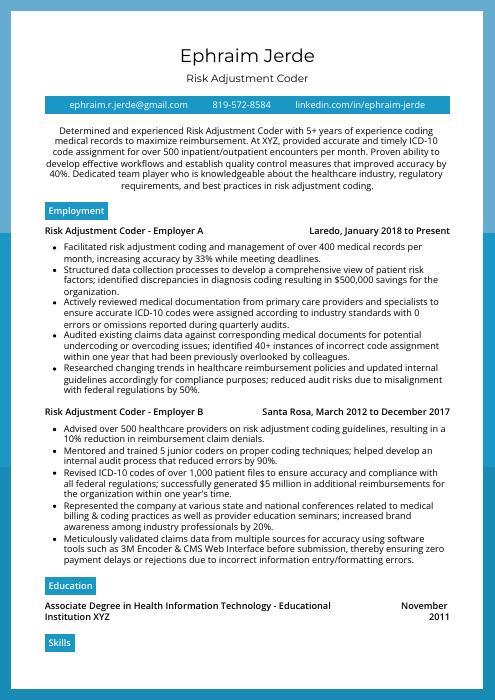 Rhea
Rhea Rezjumei
Rezjumei