Reimbursement Specialist Resume Guide
Reimbursement specialists are responsible for processing and managing payments to healthcare providers. They review insurance claims, verify the accuracy of related data, and ensure that all required documentation is in order before submitting them for payment. They also follow up on any unpaid or rejected claims to resolve discrepancies with payers.
You have an impeccable eye for detail and accuracy when it comes to filing reimbursement claims. But without a resume, employers won’t know just how valuable your skills are. To show them what you can do, write a resume that stands out from the crowd.
This guide will walk you through the entire process of creating a top-notch resume. We first show you a complete example and then break down what each resume section should look like.
Table of Contents
The guide is divided into sections for your convenience. You can read it from beginning to end or use the table of contents below to jump to a specific part.
Reimbursement Specialist Resume Sample
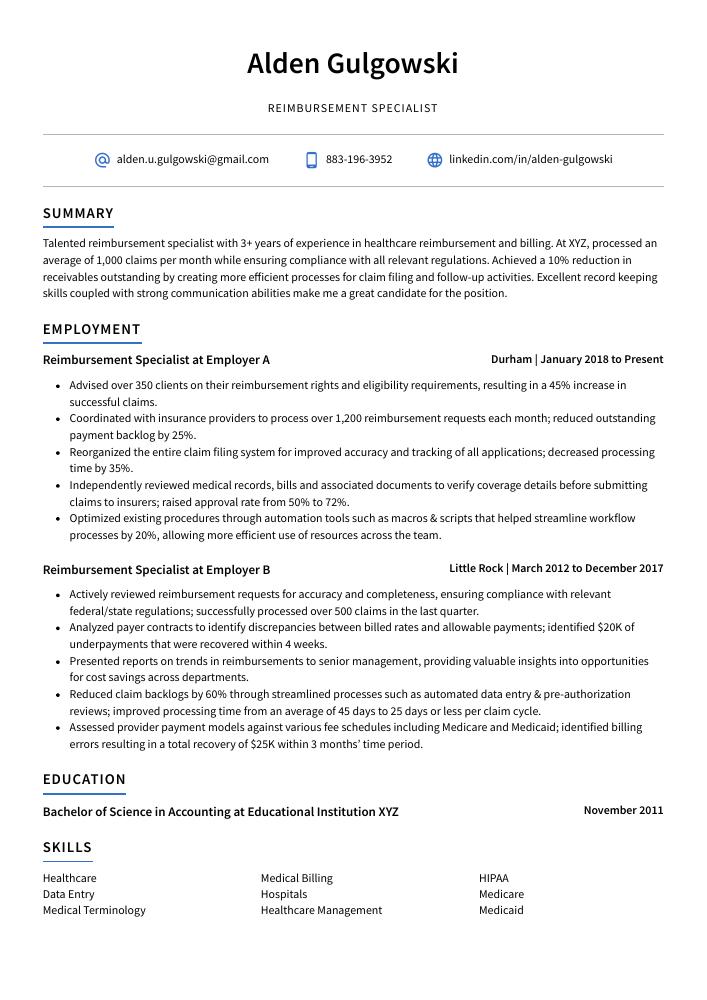
Alden Gulgowski
Reimbursement Specialist
[email protected]
883-196-3952
linkedin.com/in/alden-gulgowski
Summary
Talented reimbursement specialist with 3+ years of experience in healthcare reimbursement and billing. At XYZ, processed an average of 1,000 claims per month while ensuring compliance with all relevant regulations. Achieved a 10% reduction in receivables outstanding by creating more efficient processes for claim filing and follow-up activities. Excellent record keeping skills coupled with strong communication abilities make me a great candidate for the position.
Experience
Reimbursement Specialist, Employer A
Durham, Jan 2018 – Present
- Advised over 350 clients on their reimbursement rights and eligibility requirements, resulting in a 45% increase in successful claims.
- Coordinated with insurance providers to process over 1,200 reimbursement requests each month; reduced outstanding payment backlog by 25%.
- Reorganized the entire claim filing system for improved accuracy and tracking of all applications; decreased processing time by 35%.
- Independently reviewed medical records, bills and associated documents to verify coverage details before submitting claims to insurers; raised approval rate from 50% to 72%.
- Optimized existing procedures through automation tools such as macros & scripts that helped streamline workflow processes by 20%, allowing more efficient use of resources across the team.
Reimbursement Specialist, Employer B
Little Rock, Mar 2012 – Dec 2017
- Actively reviewed reimbursement requests for accuracy and completeness, ensuring compliance with relevant federal/state regulations; successfully processed over 500 claims in the last quarter.
- Analyzed payer contracts to identify discrepancies between billed rates and allowable payments; identified $20K of underpayments that were recovered within 4 weeks.
- Presented reports on trends in reimbursements to senior management, providing valuable insights into opportunities for cost savings across departments.
- Reduced claim backlogs by 60% through streamlined processes such as automated data entry & pre-authorization reviews; improved processing time from an average of 45 days to 25 days or less per claim cycle.
- Assessed provider payment models against various fee schedules including Medicare and Medicaid; identified billing errors resulting in a total recovery of $25K within 3 months’ time period.
Skills
- Healthcare
- Medical Billing
- HIPAA
- Data Entry
- Hospitals
- Medicare
- Medical Terminology
- Healthcare Management
- Medicaid
Education
Bachelor of Science in Accounting
Educational Institution XYZ
Nov 2011
Certifications
Certified Reimbursement Specialist
American Medical Billing Association
May 2017
1. Summary / Objective
The summary or objective at the beginning of your reimbursement specialist resume should give a brief overview of who you are and why you’re an ideal candidate for the position. Include any certifications or qualifications that make you stand out, such as experience with medical coding systems or proficiency in claims processing software. You could also mention how many years’ experience you have in this field, any awards or recognition received for outstanding performance, and how quickly customers receive reimbursements when working with you.
Below are some resume summary examples:
Proficient reimbursement specialist with 5+ years of experience in medical claims processing, auditing, and cost containment. Seeking to join ABC Health Care as a Reimbursement Specialist where I can utilize my knowledge of coding regulations and reimbursement systems to ensure accurate payments for clients. At XYZ Medical Group, identified potential savings opportunities by assessing billing data which resulted in an estimated 10% reduction in the total costs.
Diligent reimbursement specialist with 8+ years of experience in healthcare finance. Adept at understanding complex regulations and policies related to reimbursements, coding, and billing processes. Skilled communicator who works well with coworkers and clients of various backgrounds. Seeking a position as a reimbursement specialist at ABC Healthcare to help streamline financial operations while ensuring compliance with applicable laws and regulations.
Well-rounded Reimbursement Specialist with 6+ years of experience in medical billing and coding. Experienced in working with insurance companies to ensure proper reimbursement for medical services rendered. At XYZ, successfully reduced payment backlog by 30% within first 3 months on the job, saving an estimated $250k per year. Proven ability to effectively interpret complex policy regulations for accurately processing claims payments.
Professional reimbursement specialist with 4+ years of experience in a fast-paced medical office setting. Seeking to utilize expertise and knowledge of insurance policies, claim processing rules, and regulations to support the reimbursement needs at ABC Medical Center. At XYZ Clinic, managed the submission process for over 500 claims per month resulting in an average turn-around time reduction by 15%.
Hard-working and detail-oriented reimbursement specialist with 5+ years of experience. Expert in medical coding and billing, including CPT, ICD-10, HCPCS. At XYZ Hospital handled insurance claims for over 400 patients per month while keeping errors below the national average. Experienced in dealing with Medicaid/Medicare regulations to ensure timely reimbursements and compliance with government laws.
Driven reimbursement specialist with 5+ years of experience in healthcare billing and coding. Demonstrated track record of successfully optimizing reimbursements for a wide range of clients, resulting in improved cash flow for the organization. Seeking to join ABC Healthcare as a Reimbursement Specialist where I can leverage my knowledge and expertise to ensure timely payments while reducing costs.
Accomplished reimbursement specialist with 5+ years of experience in the healthcare industry. Skilled at auditing and researching medical claims, preparing financial reports, creating reimbursement worksheets to ensure accuracy of payments, and handling denials from insurance companies. Received multiple awards for 100% accuracy rate on all reimbursements processed while working at XYZ Hospital.
Detail-oriented reimbursement specialist with 5+ years of experience in a healthcare setting. Expertise in providing effective guidance for medical billing and coding, resolving payment denials, reconciling accounts receivable, and managing patient data. Looking to join ABC Medical Group as the new Reimbursement Specialist to ensure accuracy of reimbursements from insurance companies.
2. Experience / Employment
In the experience section, you’ll want to provide details on your employment history. This should be written in reverse chronological order, meaning the most recent job is listed first.
When stating what you did for each role, stick to bullet points and use action verbs such as “developed,” “analyzed,” or “implemented.” Doing so allows the reader to quickly digest what you have done and how it can benefit them if they hire you.
For example, instead of saying “Processed reimbursement requests,” you could say, “Reviewed over 500 employee expense reports per month; successfully processed 95% within 7 days while ensuring accuracy of all reimbursements.”
To write effective bullet points, begin with a strong verb or adverb. Industry specific verbs to use are:
- Processed
- Audited
- Reconciled
- Resolved
- Investigated
- Calculated
- Analyzed
- Monitored
- Updated
- Documented
- Reviewed
- Approved
- Submitted
- Tracked
Other general verbs you can use are:
- Achieved
- Advised
- Assessed
- Compiled
- Coordinated
- Demonstrated
- Developed
- Expedited
- Facilitated
- Formulated
- Improved
- Introduced
- Mentored
- Optimized
- Participated
- Prepared
- Presented
- Reduced
- Reorganized
- Represented
- Revised
- Spearheaded
- Streamlined
- Structured
- Utilized
Below are some example bullet points:
- Updated and maintained internal reimbursement databases, ensuring that all entries were accurate and up-to-date; improved data accuracy by 15%.
- Structured and processed 300+ employee reimbursement requests per month, verifying information for accuracy before payment was issued.
- Compiled detailed financial reports on a weekly basis to track reimbursements against budgeted expenditure, identifying any discrepancies of $1,000 or more; reduced overdue payments from 7 days to 2 days on average.
- Reconciled accounts with auditors quarterly in order to validate the authenticity of expense claims; identified overcharges totaling $10K which resulted in cost savings for the company.
- Thoroughly reviewed each request according to IRS regulations prior to issuing payments, maintaining compliance at all times and avoiding potential penalties or fees associated with noncompliance cases.
- Streamlined reimbursement processes for over 150 medical claims a day, resulting in an improved turnaround time of 2 days and increased efficiency by 20%.
- Developed new procedures to verify insurance information for incoming claim requests; reduced the number of errors made when processing payments by 25%.
- Improved accuracy rates from 70% to 99% on all processed reimbursement forms, ensuring timely payment was received within 1 week or less.
- Investigated discrepancies with patient records, verifying supporting documents such as doctor notes & bills before approving reimbursements; identified $5,000 worth of fraudulent activities and successfully recovered it back into company accounts last year.
- Proficiently managed online databases to track every stage in the reimbursement process: generated reports identifying any issues that delayed payments and resolved them quickly within 24 hours on average.
- Revised and audited over 500 reimbursement claims from healthcare providers, resulting in a 15% increase in accuracy and reducing errors by 10%.
- Processed up to 200 reimbursement requests daily within 24 hours; consistently maintained an average of 98% accuracy rate for all transactions.
- Meticulously reviewed patient records, insurance forms and health plan policies to ensure all data was accurate before submitting payments for approval.
- Participated in regular meetings with the accounting/finance department to discuss process improvements; implemented new procedures that improved turnaround time by 20%.
- Demonstrated expertise on medical coding systems (CPT & ICD-9) when assessing patient documentation prior to making payment reimbursements; reduced mispayment occurrences by 35%.
- Spearheaded the completion of over 300 reimbursement claims for healthcare services, resulting in a 17% decrease in processing time.
- Calculated and verified the accuracy of medical bills to ensure that all reimbursements were correct; identified and corrected any discrepancies before submitting claims.
- Tracked payment status on submitted claims using various software programs, following up with insurance companies as needed to make sure payments are received promptly; recovered over $20K in unpaid reimbursements last year.
- Resolved customer inquiries relating to claim denials or requests for additional information within 24 hours while upholding high standards of patient confidentiality at all times.
- Diligently maintained an organized filing system consisting of paper/electronic documents containing detailed records related to reimbursement cases handled during each fiscal quarter period.
- Expedited the reimbursement process for over 500+ medical and insurance claims, reducing paperwork turnaround time by 25%.
- Introduced a digital filing system which reduced errors in processing invoices by 33%, resulting in $7000 saved annually on administrative costs.
- Formulated comprehensive best practices to streamline the claim submission procedure, increasing accuracy of reimbursements paid out by 45%.
- Documented all financial transactions according to company policies and procedures; successfully identified fraudulent activities within the accounts department before they occurred.
- Consistently achieved 97% accuracy rate when verifying patient information against relevant databases, saving 3 hours per week on manual checks alone.
- Utilized advanced accounting principles to process over 300 reimbursement claims per day, ensuring accurate reimbursements and compliance with applicable laws and regulations.
- Facilitated the resolution of complex cases by interpreting policy documents, conducting in-depth analysis of documentation & data reconciliation; decreased processing backlogs by 30%.
- Represented the organization at external meetings/conferences related to financial policies & procedures as well as payment processes/procedures; successfully addressed customer concerns within 24 hours on average.
- Prepared periodic reports highlighting discrepancies or irregularities in claims submitted for reimbursement while proactively providing problem solving suggestions that improved accuracy rates from 75% to 95%.
- Competently handled a wide range of administrative duties such as verifying authorization forms, updating financial records and responding promptly to inquiries from clients within 48 hours or less.
- Mentored and trained 8 new reimbursement specialists in billing and coding processes, resulting in a 30% increase in efficient processing time.
- Audited over 5,000 medical claims to ensure they were correctly coded before submission for payment; identified incorrect submissions and corrected them with minimal expense or delay.
- Monitored the reimbursements of up to 500 clients on a monthly basis and managed follow-up actions for any discrepancies found; achieved an overall accuracy rate of 95%.
- Achieved full compliance with all government regulations governing healthcare payments by staying abreast of changes in laws, policies & procedures concerning reimbursement practices.
- Substantially reduced rejections from insurance providers due to improper coding or filing errors by utilizing sophisticated software tools used for accurate claim validation & submission cycles.
- Submitted over 500 reimbursement claims a month for medical, dental and other expenses; accurately tracked claim statuses to ensure timely payments to clients.
- Approved an average of 95% of daily submitted claims within 24 hours; saved the company over $200,000 in unnecessary payment delays by streamlining processes.
- Reliably processed high volumes of paperwork with 100% accuracy while adhering to all internal policies and government regulations regarding filing procedures & deadlines.
- Reviewed discrepancies between invoices and insurance documents every day; identified errors quickly leading to reduced rejections/denials rate by 15%.
3. Skills
Skill requirements will differ from employer to employer – this can easily be determined via the job advert. Organization ABC may require the candidate to be proficient with QuickBooks, while Organization XYZ might want someone who is knowledgeable of Microsoft Excel.
It is important to tailor the skills section of your resume for each job you are applying for because many employers use applicant tracking systems these days. These computer programs scan resumes for certain keywords before passing them on to a human.
Once listed here, you can further elaborate on your abilities by discussing it in more detail in other areas such as the summary or experience section.
Below is a list of common skills & terms:
- Access
- Accounts Receivable
- CPT
- Clinical Research
- Customer Satisfaction
- Data Entry
- EHR
- EMR
- Epic Systems
- HIPAA
- Health Insurance
- Healthcare
- Healthcare Information Technology
- Healthcare Management
- Healthcare Reimbursement
- Hospitals
- Insurance
- Invoicing
- Managed Care
- Medicaid
- Medical Billing
- Medical Coding
- Medical Records
- Medical Terminology
- Medicare
- Process Improvement
- Revenue Cycle
- Team Leadership
- Teamwork
- Time Management
- U.S. Health Insurance Portability and Accountability Act
4. Education
Including an education section on your resume will depend on how far along you are in your career. If you just graduated and have no prior experience, mention your education below the resume objective. However, if you have years of experience as a reimbursement specialist, it might be more beneficial to omit the education section altogether so that employers can focus more on relevant work history instead.
If including an education section is necessary for the job application process, try to highlight courses or subjects related to medical billing and coding which are typically required for this role.
Bachelor of Science in Accounting
Educational Institution XYZ
Nov 2011
5. Certifications
Certifications are a great way to demonstrate your expertise in a specific field. They show potential employers that you have taken the time and effort to become proficient in an area related to their job opening, which can give you an edge over other applicants.
Including certifications on your resume is especially beneficial if they are relevant or required for the position you are applying for. Doing so will help prove that you have the necessary skills and qualifications needed for success in this role.
Certified Reimbursement Specialist
American Medical Billing Association
May 2017
6. Contact Info
Your name should be the first thing a reader sees when viewing your resume, so ensure its positioning is prominent. Your phone number should be written in the most commonly used format in your country/city/state, and your email address should be professional.
You can also choose to include a link to your LinkedIn profile, personal website, or other online platforms relevant to your industry.
Finally, name your resume file appropriately to help hiring managers; for Alden Gulgowski, this would be Alden-Gulgowski-resume.pdf or Alden-Gulgowski-resume.docx.
7. Cover Letter
Attaching a cover letter to your job application can be a great way to make yourself stand out. It is usually composed of 2 to 4 paragraphs and allows you the opportunity to explain why you are an excellent fit for the role in more detail than what is mentioned in your resume.
Cover letters give recruiters and hiring managers valuable insights into who you are as a professional, allowing them to form a better opinion of your qualifications and skillset. Although not all jobs will require one, writing one might increase your chances of getting noticed by potential employers.
Below is an example cover letter:
Dear Marcel,
I am writing to apply for the position of Reimbursement Specialist at XYZ Company. I am a highly motivated professional with over 10 years of experience in billing and coding, as well as insurance reimbursement. My expertise lies in providing support to patients and families regarding their medical bills and claims. In addition, I have a strong background in customer service, which has helped me build positive relationships with both patients and insurance companies.
In my current role as a Reimbursement Specialist at ABC Company, I handle all aspects of patient billing and collections. This includes preparing invoices, submitting claims to insurance companies, following up on outstanding payments, and resolving any discrepancies. I have been successful in reducing our accounts receivable by 15% over the past year through effective negotiations with insurance companies and improved collection efforts. In addition, I provide excellent customer service to our patients by answering their questions regarding their bill or claim status in a timely manner.
I believe that my skills and experience would be an asset to your team at XYZ Company. I am eager to utilize my knowledge in order to contribute to the success of your organization. Thank you for your time and consideration; I look forward to speaking with you soon about this opportunity.
Sincerely,
Alden
Reimbursement Specialist Resume Templates
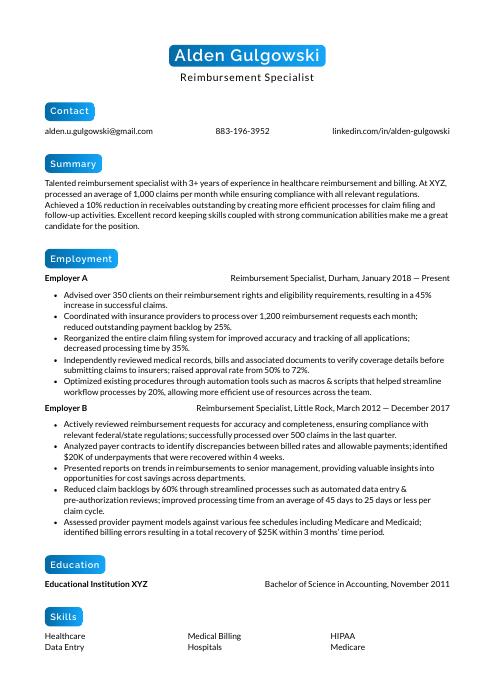 Kinkajou
Kinkajou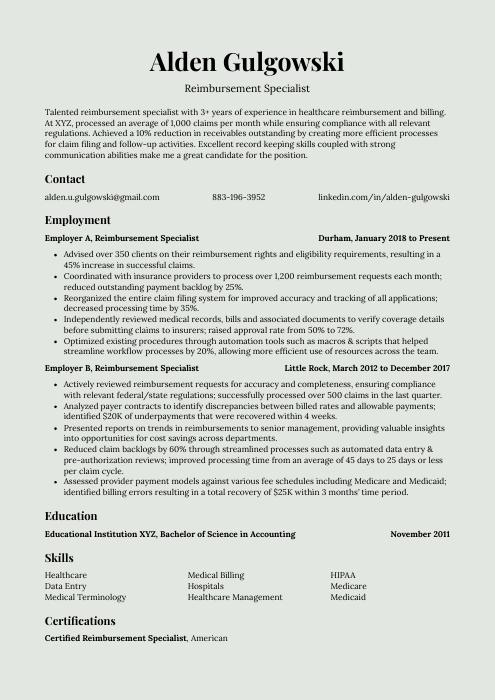 Saola
Saola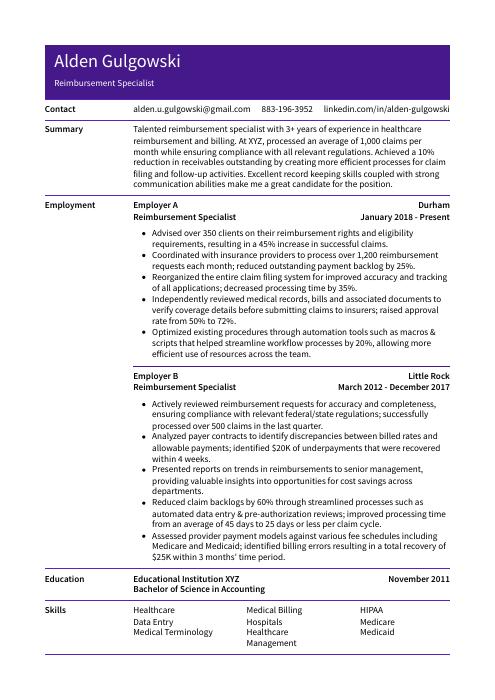 Pika
Pika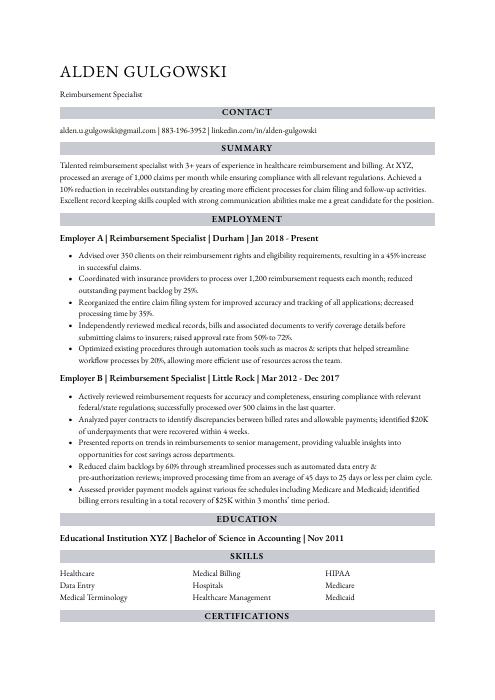 Numbat
Numbat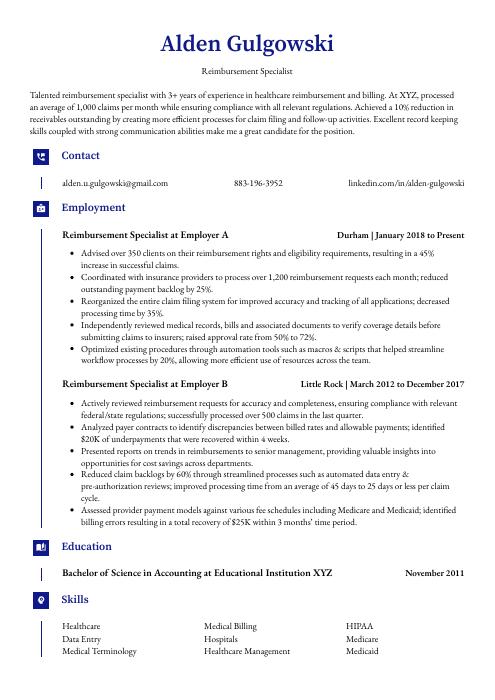 Gharial
Gharial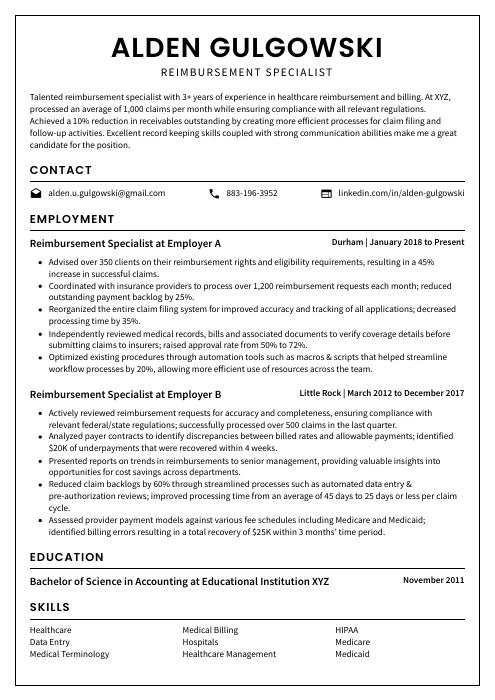 Cormorant
Cormorant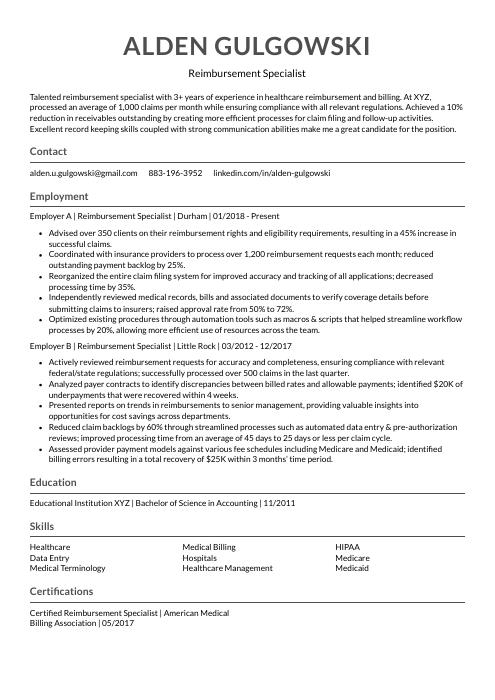 Indri
Indri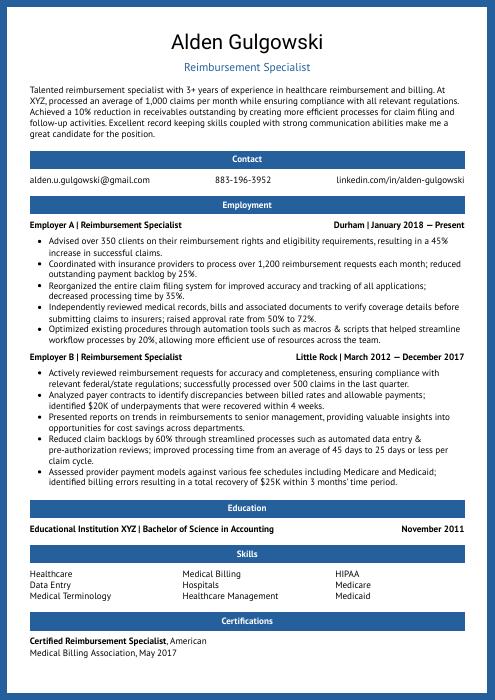 Ocelot
Ocelot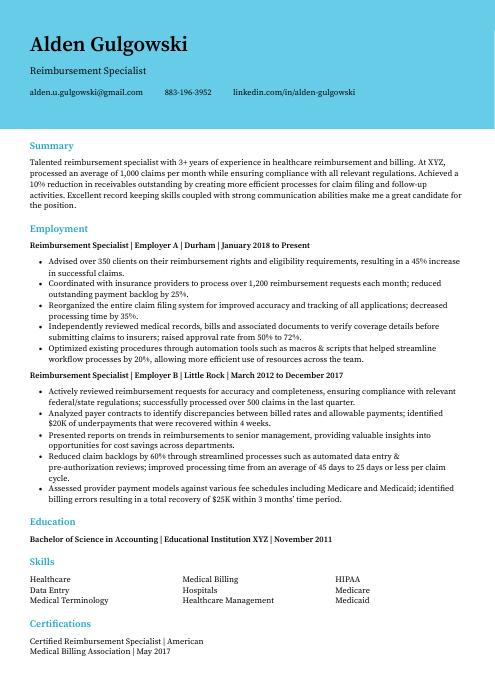 Dugong
Dugong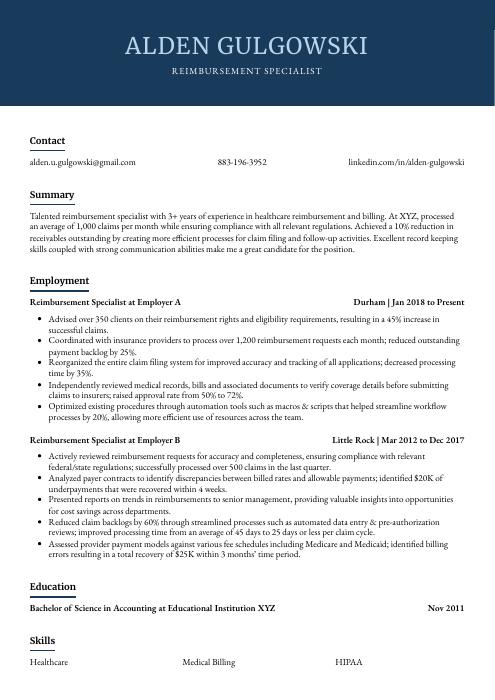 Bonobo
Bonobo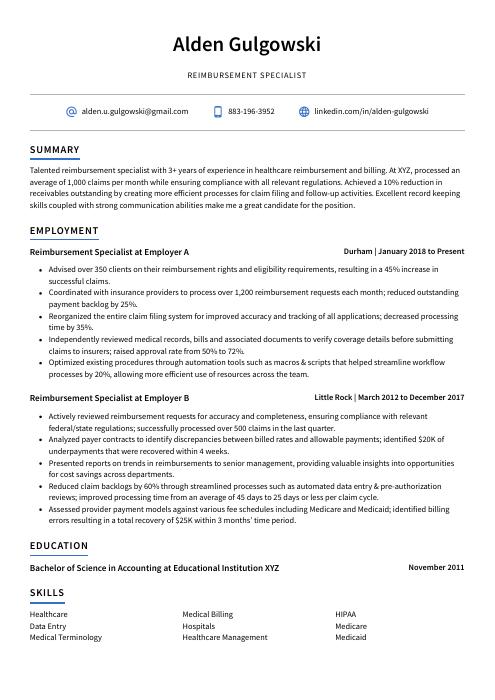 Axolotl
Axolotl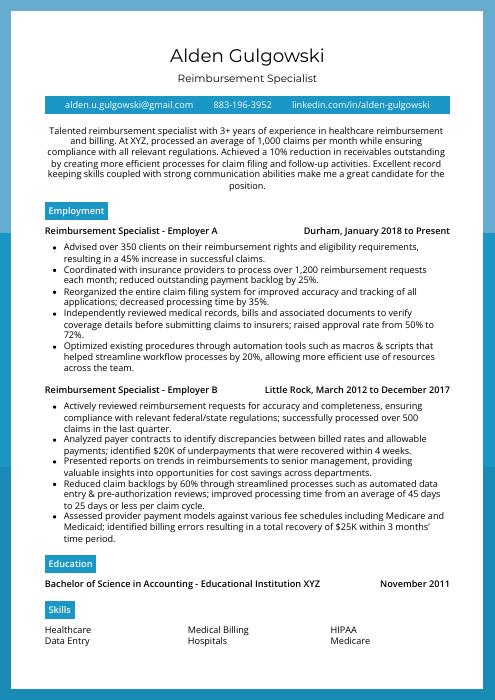 Rhea
Rhea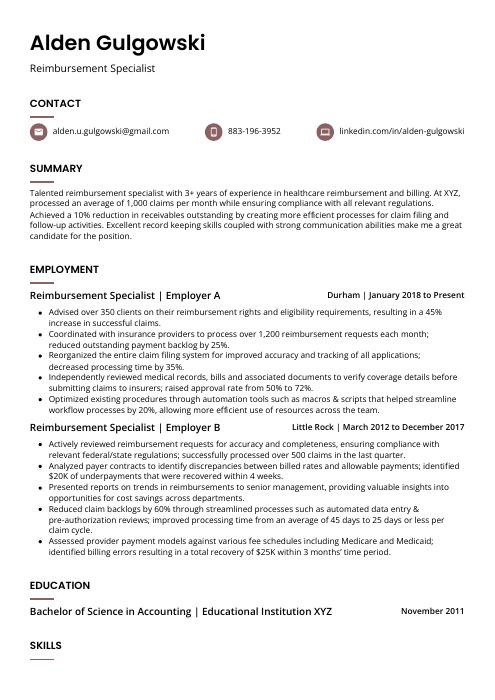 Fossa
Fossa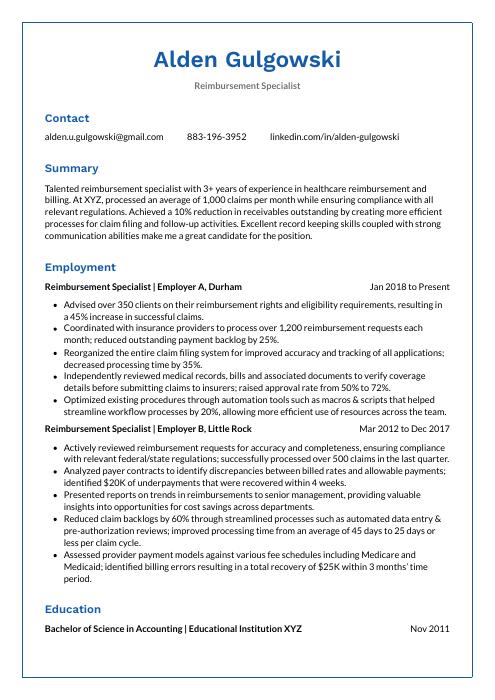 Markhor
Markhor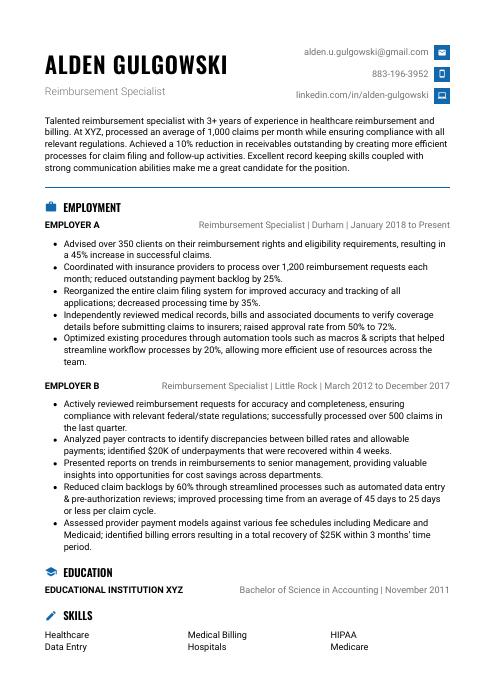 Echidna
Echidna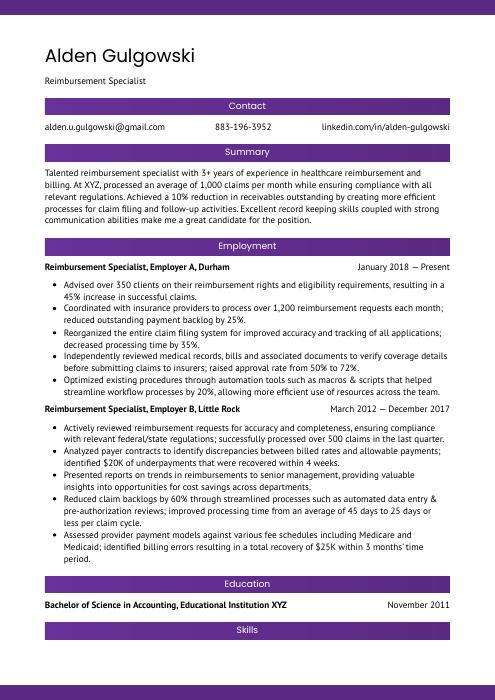 Jerboa
Jerboa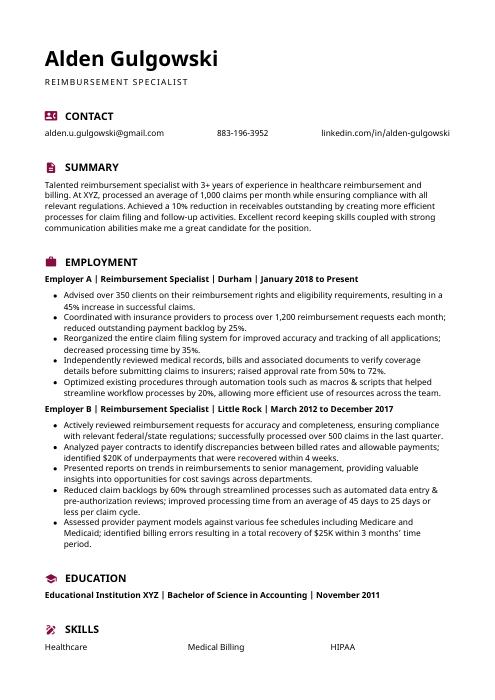 Hoopoe
Hoopoe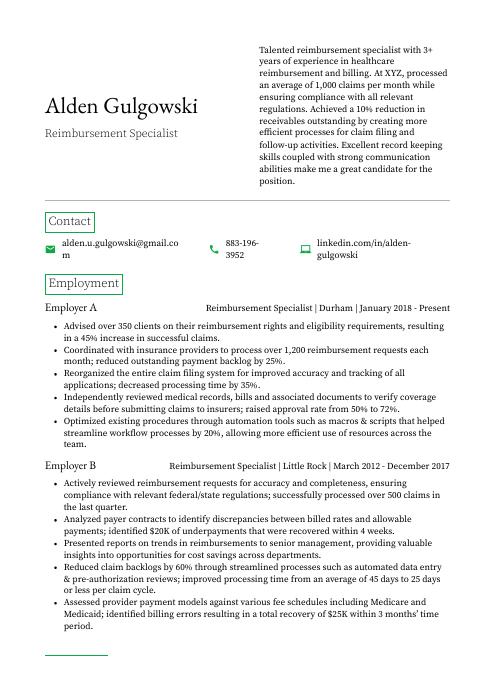 Quokka
Quokka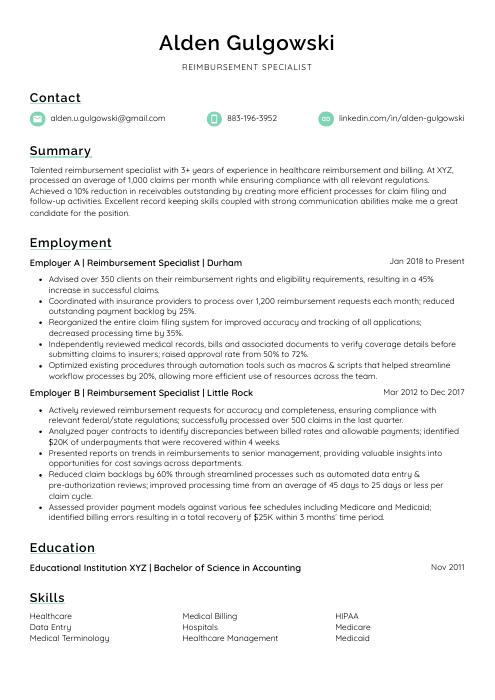 Lorikeet
Lorikeet Rezjumei
Rezjumei