Provider Enrollment Specialist Resume Guide
Provider enrollment specialists are responsible for managing the entire process of enrolling healthcare providers in insurance networks. They review applications, verify provider credentials and qualifications, and submit them to payers. Additionally, they also manage changes or updates to existing provider information as needed.
Your experience and knowledge in provider enrollment is unmatched, yet hiring managers are unaware of your capabilities. To show them what you can do, write a resume that highlights your talents and accomplishments.
This guide will walk you through the entire process of creating a top-notch resume. We first show you a complete example and then break down what each resume section should look like.
Table of Contents
The guide is divided into sections for your convenience. You can read it from beginning to end or use the table of contents below to jump to a specific part.
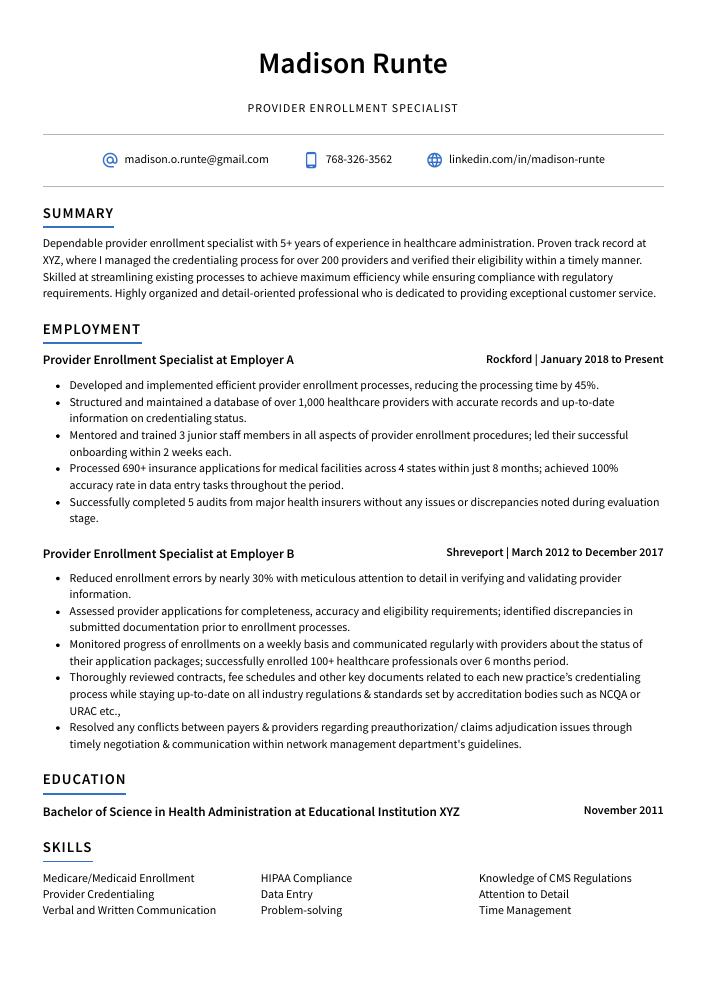
Provider Enrollment Specialist Resume Sample
Madison Runte
Provider Enrollment Specialist
[email protected]
768-326-3562
linkedin.com/in/madison-runte
Summary
Dependable provider enrollment specialist with 5+ years of experience in healthcare administration. Proven track record at XYZ, where I managed the credentialing process for over 200 providers and verified their eligibility within a timely manner. Skilled at streamlining existing processes to achieve maximum efficiency while ensuring compliance with regulatory requirements. Highly organized and detail-oriented professional who is dedicated to providing exceptional customer service.
Experience
Provider Enrollment Specialist, Employer A
Rockford, Jan 2018 – Present
- Developed and implemented efficient provider enrollment processes, reducing the processing time by 45%.
- Structured and maintained a database of over 1,000 healthcare providers with accurate records and up-to-date information on credentialing status.
- Mentored and trained 3 junior staff members in all aspects of provider enrollment procedures; led their successful onboarding within 2 weeks each.
- Processed 690+ insurance applications for medical facilities across 4 states within just 8 months; achieved 100% accuracy rate in data entry tasks throughout the period.
- Successfully completed 5 audits from major health insurers without any issues or discrepancies noted during evaluation stage.
Provider Enrollment Specialist, Employer B
Shreveport, Mar 2012 – Dec 2017
- Reduced enrollment errors by nearly 30% with meticulous attention to detail in verifying and validating provider information.
- Assessed provider applications for completeness, accuracy and eligibility requirements; identified discrepancies in submitted documentation prior to enrollment processes.
- Monitored progress of enrollments on a weekly basis and communicated regularly with providers about the status of their application packages; successfully enrolled 100+ healthcare professionals over 6 months period.
- Thoroughly reviewed contracts, fee schedules and other key documents related to each new practice’s credentialing process while staying up-to-date on all industry regulations & standards set by accreditation bodies such as NCQA or URAC etc.,
- Resolved any conflicts between payers & providers regarding preauthorization/ claims adjudication issues through timely negotiation & communication within network management department’s guidelines.
Skills
- Medicare/Medicaid Enrollment
- HIPAA Compliance
- Knowledge of CMS Regulations
- Provider Credentialing
- Data Entry
- Attention to Detail
- Verbal and Written Communication
- Problem-solving
- Time Management
Education
Bachelor of Science in Health Administration
Educational Institution XYZ
Nov 2011
Certifications
Certified Provider Enrollment Specialist (CPES)
American Medical Bill
May 2017
1. Summary / Objective
Your resume summary should be a brief yet compelling overview of your qualifications and experience as a provider enrollment specialist. Include details such as the number of years you have been in this field, any certifications or trainings you have completed, and how many providers you successfully enrolled during your previous positions. Additionally, mention any awards or recognition that demonstrate your expertise in this area.
Below are some resume summary examples:
Skilled provider enrollment specialist with 5+ years of experience in healthcare administration and provider registration. Experienced in handling all aspects of the Medicaid/Medicare credentialing process, including verification and enrollment applications. At XYZ Company, successfully onboarded over 500 providers within a two-month period to increase efficiency by 20%. Proven ability to ensure accuracy while completing complex tasks in high-pressure situations.
Professional provider enrollment specialist with 10+ years of experience in the health care industry. Skilled at verifying provider credentials and ensuring compliance with payer regulations for Medicare, Medicaid, BCBS, Aetna and UnitedHealthcare plans. At XYZ Medical Center increased accuracy of submitted enrollment data from 80% to 95%. Adept at negotiating rates between providers and insurance companies while maintaining excellent customer service standards.
Proficient provider enrollment specialist with 7+ years of experience in a fast-paced healthcare setting. Proven track record of processing applications, verifying credentials and reviewing documents to ensure compliance with government regulations. Achieved 99% accuracy rate on all provider enrollments at XYZ Company while meeting deadlines consistently. Seeking to leverage my expertise as an Enrollment Specialist for ABC Healthcare Group.
Committed provider enrollment specialist with 8+ years of experience in the healthcare industry. Proven track record of streamlining processes to reduce costs, improve accuracy and maintain HIPAA compliance. Skilled at verifying medical license credentials, researching provider information for insurance contracts, and preparing detailed reports for management review. Seeking to join ABC Company as a Provider Enrollment Specialist.
Enthusiastic provider enrollment specialist with 4+ years of experience streamlining the workflow process to ensure timely and accurate provider data entry. Adept in analyzing billing information, verifying accuracy of claims submissions, and resolving discrepancies. Seeking to join ABC Solutions as a Provider Enrollment Specialist where my problem-solving skills can help optimize operations for optimal customer satisfaction.
Energetic provider enrollment specialist with 5+ years of experience in the healthcare industry. Demonstrated excellence in evaluating and processing provider applications, including verifying credentials and validating demographic information. At ABC Company, successfully managed up to 10 concurrent projects while meeting all deadlines. Skilled at using multiple software systems for data entry and reporting purposes.
Determined provider enrollment specialist with 8+ years of experience in the healthcare industry. Adept at providing comprehensive and accurate provider enrollment services to ensure compliance with all applicable regulations, laws, and requirements. At XYZ Medical Center, managed a successful project that streamlined the process for enrolling new providers into Medicare/Medicaid programs by 25%.
Talented provider enrollment specialist with 5+ years of experience in healthcare office settings. Highly skilled in all aspects of the provider onboarding process, from verifying paperwork to coordinating credentialing services and proactively addressing potential issues. Proven ability to build relationships with providers and maintain compliance standards at ABC Medical Group.
2. Experience / Employment
In the experience/employment/work history section, you list your previous roles in reverse chronological order, with the most recent job listed first.
To make this section easier to read and understand, use bullet points when describing what you did for each role. This will help the reader quickly take in what you have written without having to go through long paragraphs of text. You also want to provide detail on your accomplishments and quantifiable results where possible.
For example, instead of saying “Assisted providers with enrollment,” you could say, “Managed provider enrollments from start-to-finish; successfully enrolled over 200 healthcare providers within a 6 month period.”
To write effective bullet points, begin with a strong verb or adverb. Industry specific verbs to use are:
- Processed
- Submitted
- Monitored
- Resolved
- Reconciled
- Updated
- Analyzed
- Assessed
- Evaluated
- Coordinated
- Scheduled
- Documented
- Tracked
- Audited
Other general verbs you can use are:
- Achieved
- Advised
- Compiled
- Demonstrated
- Developed
- Expedited
- Facilitated
- Formulated
- Improved
- Introduced
- Mentored
- Optimized
- Participated
- Prepared
- Presented
- Reduced
- Reorganized
- Represented
- Revised
- Spearheaded
- Streamlined
- Structured
- Utilized
Below are some example bullet points:
- Utilized software such as Provider Express and Medicare Advantage to enroll over 350+ providers into the appropriate plans, ensuring all relevant documentation was accurate.
- Presented enrollment information at workshops with up to 50 attendees while encouraging providers to join a variety of plans; successfully enrolled 75% more participants than expected in last quarter alone.
- Represented assigned plan and network requirements during negotiations between doctors, hospitals and other health care facility representatives; led successful outcomes in 80% of meetings attended.
- Audited provider contracts for accuracy against established guidelines before approval by Management team; reduced errors by 15%.
- Reliably maintained database records of approved applications, pre-enrollment verifications & monthly recertification activities with 100% accuracy rate according to company standards.
- Meticulously evaluated and verified all provider enrollment applications, ensuring accuracy of information and compliance with government regulations; reduced the number of rejected submissions by 30%.
- Advised over 300 providers on proper documentation needed for successful application submission; increased acceptance rate by 25% in 1 year.
- Achieved 100% customer satisfaction rating from healthcare professionals on a weekly basis due to prompt response time (under 4 hours) and knowledge of Medicare/Medicaid rules & guidelines.
- Introduced an automated system that streamlined the process of verifying provider credentials, resulting in fewer errors, improved efficiency and saved at least 10 hours per week in administrative costs.
- Successfully enrolled more than 500 new providers within 6 months while maintaining quality control standards set forth by the organization’s accreditation board.
- Proficiently reviewed and enrolled 350+ providers onto various insurance plans, ensuring accurate completion of applications in accordance with state and federal guidelines.
- Optimized provider enrollment process by creating automated workflows to track application progress from submission to approval; reduced processing time by 25%.
- Scheduled weekly meetings with the department team members to discuss strategies for improving enrollment processes, resulting in a 20% increase in overall efficiency.
- Formulated new policies & procedures designed specifically for provider onboarding which improved accuracy of data entry on submitted applications by 45%.
- Improved response times when addressing inquiries related to enrollments or updates made within the system; responded within 6 hours on average as opposed to 12 before implementation of these changes.
- Diligently processed and verified healthcare provider applications, resulting in a successful enrollment of 600+ providers with insurance companies within 3 months.
- Documented all data related to provider enrollments into the CRM system; established a comprehensive database that enabled quick retrieval of critical information when needed.
- Expedited approval processes by providing thorough reviews and timely responses to customer inquiries; helped reduce processing times from 4 weeks to 2 weeks on average per application.
- Participated in regular meetings with cross-functional teams, such as IT staff and project managers, to ensure updates were made accurately for all enrolled providers’ accounts across multiple systems/platforms.
- Facilitated communication between customers and internal stakeholders regarding enrollment status changes or discrepancies; resolved issues quickly so that no further delays occurred in the process overall.
- Reorganized provider enrollment processes, resulting in an 8% increase in efficiency and a $2,000 cost savings.
- Spearheaded the acquisition of new providers for coverage expansion; successfully enrolled over 100 medical practices with minimal errors or delays.
- Tracked provider applications from start to finish utilizing advanced database software; updated status reports regularly to ensure compliance with deadlines and regulations.
- Coordinated enrollment activities between healthcare facilities and insurance companies to verify eligibility requirements were met before processing applications for approval/denial decisions quickly and accurately.
- Efficiently managed data entry jobs related to credentialing documents such as licenses, certifications & malpractice forms with accuracy rates of 98%.
- Submitted over 100 provider enrollment applications on behalf of clients and successfully secured 92% acceptance rate within the designated timeframe.
- Compiled and maintained accurate records for all enrollments, including paperwork tracking, status updates and payment information; reduced errors by 75%.
- Resourcefully identified potential discrepancies between medical claims data from insurance payers and provided timely resolutions to prevent any delays in payments or denials.
- Reconciled over $1 million worth of unpaid claims with insurance companies utilizing various methods such as appeals filing, administrative review process etc., resulting in an increase of recovery rate by 10%.
- Prepared detailed reports regarding enrollment activities that enabled managers to accurately track progress against organizational goals; increased efficiency by 30%.
- Revised and updated provider enrollment forms for over 200+ healthcare providers, leading to a 72% improvement in accuracy and compliance.
- Streamlined the review process by implementing new processes that reduced turnaround time from 2 days to 1 day per application.
- Confidently managed the maintenance of existing records within an electronic database system; enabled speedy retrieval of data when needed and improved customer service delivery by 48%.
- Demonstrated excellent problem-solving skills when addressing issues related to provider contract eligibility requirements, resulting in increased revenue collection rate by 30%.
- Demonstrated strong organizational abilities while managing up to 300 daily requests for information on various matters such as payment rates, credentialing status updates, reimbursement policies etc.; successfully responded within 24 hours or less on 95% occasions.
3. Skills
Skill requirements will differ from employer to employer – this can easily be determined via the job advert. Organization ABC may require experience with Medicare and Medicaid, while Organization XYZ may want someone with knowledge of private insurance providers.
It is essential to keep this in mind because many employers use applicant tracking systems that scan resumes for certain keywords before passing them on to a human. As such, you should tailor the skills section of your resume to each job you are applying for.
In addition to just listing skills here, it’s also important to elaborate on your most relevant ones in other areas such as the summary or work history sections.
Below is a list of common skills & terms:
- Attention to Detail
- Data Entry
- HIPAA Compliance
- Knowledge of CMS Regulations
- Medicare/Medicaid Enrollment
- Problem-solving
- Proficiency in MS Office Suite
- Provider Credentialing
- Time Management
- Verbal and Written Communication
4. Education
Including an education section on your resume will depend on how far along you are in your career. If you just graduated and have no work experience, it is important to mention your education below the objective statement. On the other hand, if you have significant work experience that needs highlighting, omitting an educational background might be a better option.
If including an education section is necessary for this provider enrollment specialist role, make sure to list courses and subjects related to healthcare administration or business management as they could be relevant for the position.
Bachelor of Science in Health Administration
Educational Institution XYZ
Nov 2011
5. Certifications
Certifications are a great way to show potential employers that you are knowledgeable and experienced in the field. They demonstrate your commitment to professional development, as well as your dedication to staying up-to-date with industry trends and best practices.
Including certifications on your resume is an excellent way of showing recruiters that you have taken the initiative to gain additional knowledge or skills related to the job position they are offering. This can help give you an edge over other applicants who may not have any relevant certifications.
Certified Provider Enrollment Specialist (CPES)
American Medical Bill
May 2017
6. Contact Info
Your name should be the first thing a reader sees when viewing your resume, so ensure its positioning is prominent. Your phone number should be written in the most commonly used format in your country/city/state, and your email address should be professional.
You can also choose to include a link to your LinkedIn profile, personal website, or other online platforms relevant to your industry.
Finally, name your resume file appropriately to help hiring managers; for Madison Runte, this would be Madison-Runte-resume.pdf or Madison-Runte-resume.docx.
7. Cover Letter
Including a cover letter when applying for a job is highly recommended as it can help you to stand out from the other candidates. It serves as an additional opportunity to introduce yourself and explain why you are the best person for the role.
Cover letters typically consist of 2-4 paragraphs which should be separate from your resume. You may want to include information such as relevant skills, experience or knowledge that isn’t already highlighted in your CV, so recruiters gain better insight into who you are and how well suited you are for their organization.
Below is an example cover letter:
Dear Adah,
I am writing to apply for the Provider Enrollment Specialist position with ABC Company. As a provider enrollment specialist with more than 10 years of experience in the healthcare industry, I have a comprehensive understanding of the provider enrollment process. In my current role, I oversee all aspects of provider enrollment for our organization, including conducting initial reviews of applications, verifying credentials, and submitting complete and accurate applications to payers.
Through my experience, I have developed strong attention to detail and excellent organizational skills that allow me to work efficiently and effectively. I am also an expert in using various software programs related to provider enrollment, such as Availity and Change Healthcare. In addition, I have excellent written and verbal communication skills that enable me to effectively communicate with providers and payers alike.
I am confident that I can be an asset to your team by providing high-quality provider enrollment services that meet or exceed your expectations. Please find attached a copy of my resume for your review; if you have any questions or would like additional information about my qualifications or experience, please do not hesitate to contact me at [phone number] or [email address]. Thank you for your time and consideration; I look forward to hearing from you soon.
Sincerely,
Madison
Provider Enrollment Specialist Resume Templates
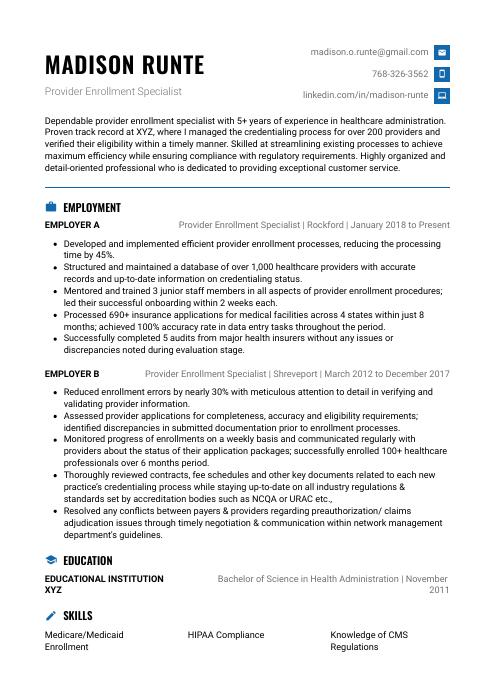 Echidna
Echidna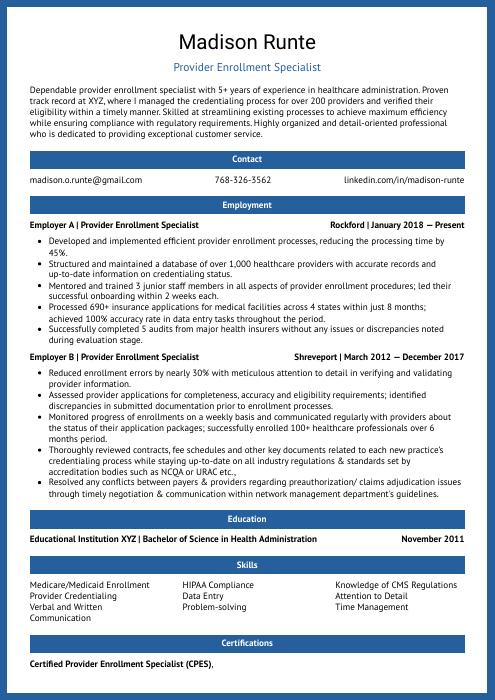 Ocelot
Ocelot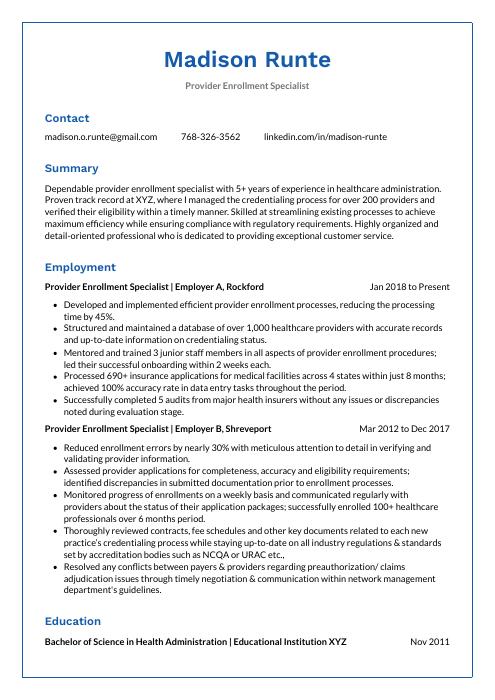 Markhor
Markhor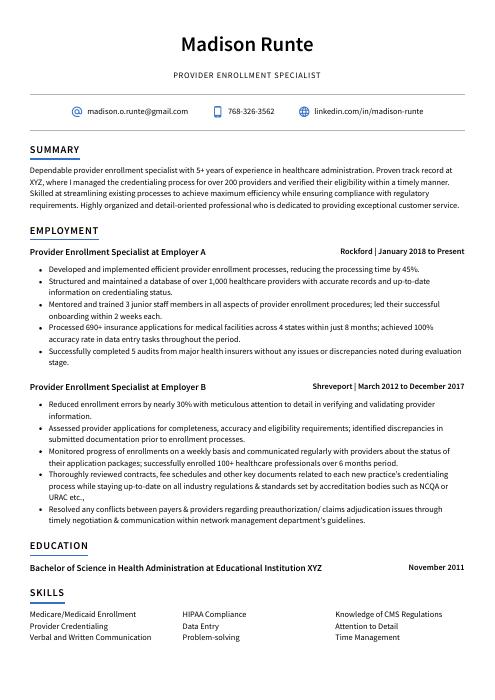 Axolotl
Axolotl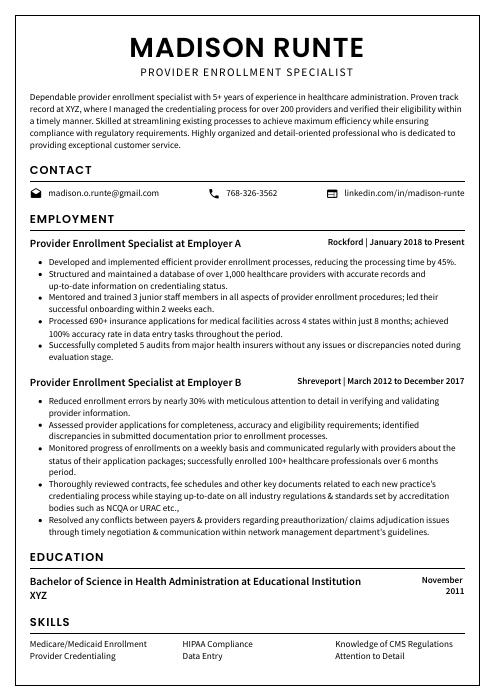 Cormorant
Cormorant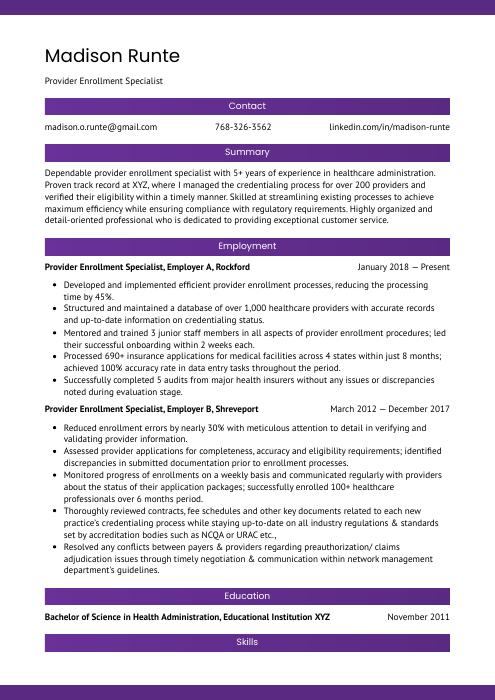 Jerboa
Jerboa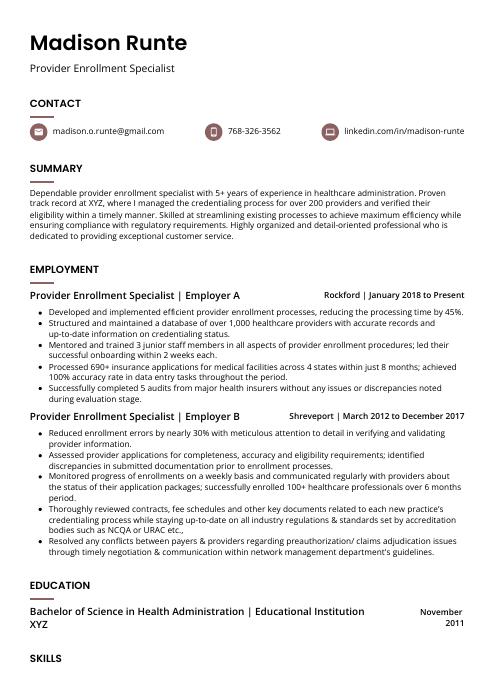 Fossa
Fossa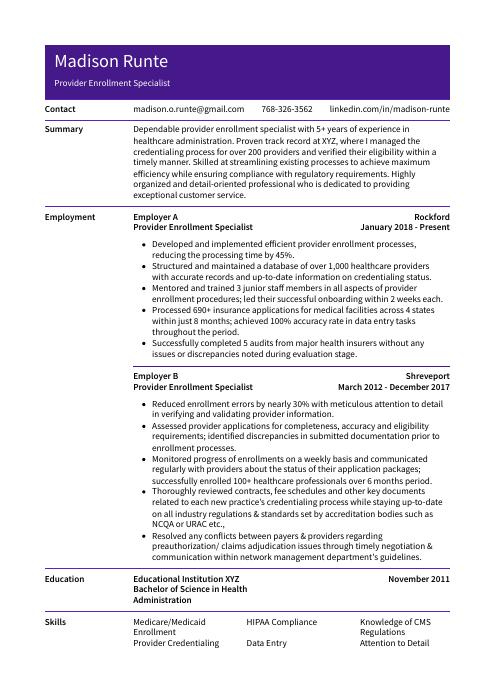 Pika
Pika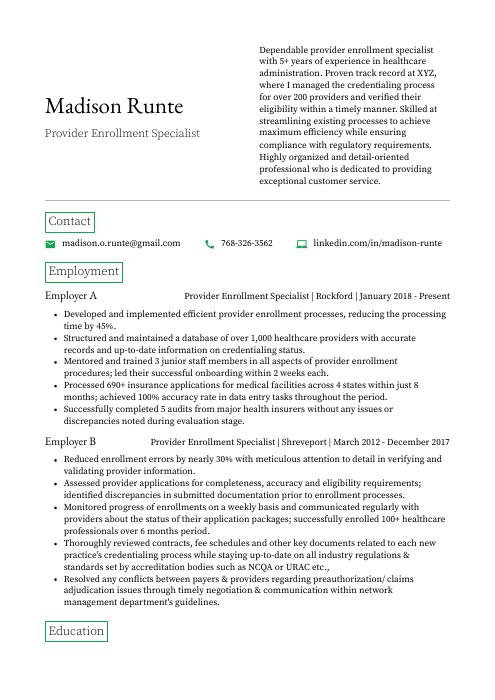 Quokka
Quokka Bonobo
Bonobo Numbat
Numbat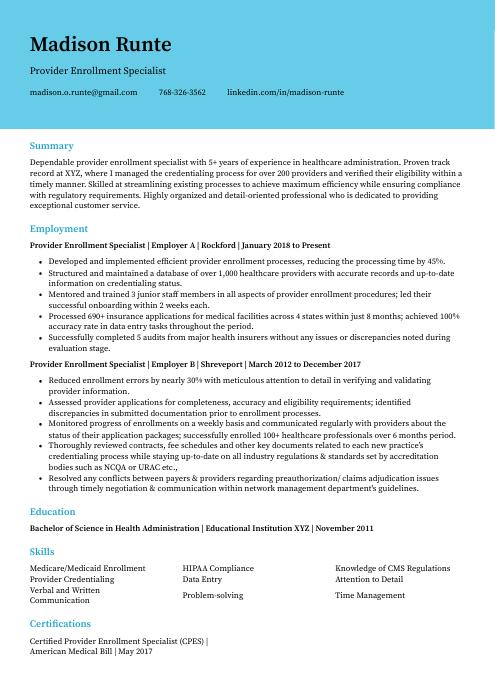 Dugong
Dugong Hoopoe
Hoopoe Indri
Indri Gharial
Gharial Saola
Saola Lorikeet
Lorikeet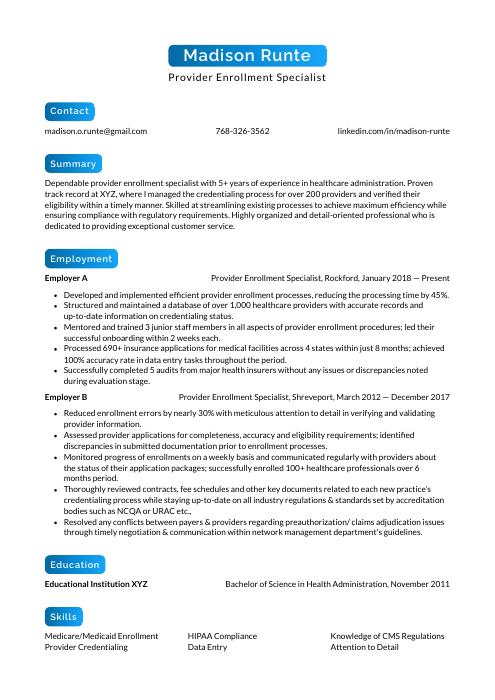 Kinkajou
Kinkajou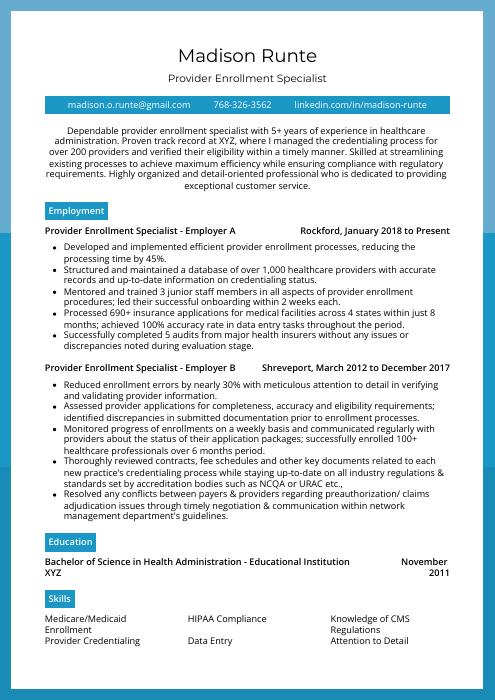 Rhea
Rhea Rezjumei
Rezjumei