Claims Analyst Resume Guide
Claims analysts review and analyze insurance claims to determine the legitimacy of a claim. They use technical knowledge, investigative skills, and experience to assess whether or not an insurer should pay out on a particular claim. Claims analysts also identify fraudulent activities in order to protect companies from financial loss.
Your analytical skills and experience in the insurance industry make you a perfect fit for any claims analyst job. To get noticed by employers, you must create an eye-catching resume that highlights your expertise.
This guide will walk you through the entire process of creating a top-notch resume. We first show you a complete example and then break down what each resume section should look like.
Table of Contents
The guide is divided into sections for your convenience. You can read it from beginning to end or use the table of contents below to jump to a specific part.
Claims Analyst Resume Sample
Abdiel Kautzer
Claims Analyst
[email protected]
329-302-7533
linkedin.com/in/abdiel-kautzer
Summary
Diligent and detail-oriented claims analyst with 5+ years of experience providing accurate and timely settlement solutions for a wide range of clients. Proven record of successfully assessing claim validity, investigating facts, and managing dispute resolution processes within established guidelines. Seeking to join ABC Insurance as an integral part in the Claims Department by leveraging strong analytical skills and customer service acumen.
Experience
Claims Analyst, Employer A
Louisville, Jan 2018 – Present
- Reorganized and streamlined the claims process to reduce processing time by 25%, resulting in an overall cost savings of $15,000.
- Assessed and evaluated over 600 insurance claim applications within a given timeframe while adhering to strict company guidelines and regulations; maintained an accuracy rate of 93%.
- Presented findings on 8 major accident cases at corporate meetings, outlining viable solutions that minimized costs for all parties involved.
- Consistently achieved superior customer satisfaction ratings with regards to client handling skills and thoroughness of claims analysis; received 3 commendations from customers in the last quarter alone.
- Advised new team members on best practices when dealing with complex medical or technical insurance claim inquiries, increasing productivity by 10%.
Claims Analyst, Employer B
Durham, Mar 2012 – Dec 2017
- Streamlined claims processing by analyzing and reorganizing existing procedures, resulting in a 20% decrease in average time to process claims.
- Evaluated approximately 500 medical insurance claim forms per month for accuracy, completeness, and compliance with established regulations; identified $10K of fraudulent activity within the first quarter of employment.
- Meticulously examined all documents associated with each claim before making decisions on payment approval or denial; maintained an accuracy rate of 95%.
- Mentored junior analysts on proper procedure when assessing incoming claims as part of onboarding program; reduced training costs by 15%.
- Developed clear guidelines to be used when handling disputes between claimants/insurers and resolving conflicting information efficiently; improved customer satisfaction ratings by 10 points over 6 months period.
Skills
- Insurance
- Time Management
- Claim
- Data Entry
- Claims Management
- Teamwork
- Healthcare
- Process Improvement
- Customer Satisfaction
Education
Bachelor of Science in Business Administration
Educational Institution XYZ
Nov 2011
Certifications
Certified Professional Claims Analyst
Claims and Litigation Management Alliance (
May 2017
1. Summary / Objective
A resume summary/objective is like a movie trailer – it should give the employer an overview of who you are and why they should hire you as their claims analyst. In this section, emphasize your qualifications such as any certifications or degrees related to insurance and risk management, the number of years’ experience in analyzing complex claims data, and how you have successfully resolved customer disputes.
Below are some resume summary examples:
Enthusiastic and detail-driven claims analyst with 4+ years of experience in the insurance industry. At XYZ, successfully identified fraudulent activity on over 500 claims resulting in a savings of $1.2M annually. Skilled at analyzing complex healthcare data to assess risk and ensure accuracy while meeting tight deadlines. Adept at process improvement initiatives that reduce costs while maintaining quality service levels for policyholders.
Well-rounded claims analyst with 5+ years of experience in the insurance industry. Possesses a comprehensive understanding of policies and regulations, as well as an aptitude for problem-solving. Seeking to join ABC Insurance Company where I can apply my expertise to ensure excellent customer service and effective claims management. At XYZ, achieved 97% accuracy rate in auditing processes while reducing processing time by 28%.
Energetic and organized claims analyst with five years of experience in the insurance industry. At XYZ, managed and processed up to 1,000+ claims per month for a variety of insurance products such as auto, property damage, worker’s compensation and liability policies from inception through closure. Skilled at identifying fraudulent or inaccurate data on policy documents while ensuring customer satisfaction is met every time.
Hard-working and detail-oriented claims analyst with 5+ years of experience in reviewing and processing insurance claims. Committed to providing excellent customer service while striving for accurate resolution of complex cases. At Company X, successfully processed over 1,000 claims per month without any errors or omissions. Seeking to join ABC Insurance as a Claims Analyst to utilize my expertise in the field.
Seasoned claims analyst with 8+ years of experience in the insurance industry. At XYZ, successfully managed over 1000 customer accounts and achieved a 92% rate of successful claim resolution. Received recognition for consistently exceeding expectations on customer satisfaction surveys by 7%. Skilled at quickly assessing complex situations to determine best possible solutions while adhering to legal guidelines.
Reliable and analytical claims analyst with six years of experience in the insurance industry. Seeking to leverage expertise in data analysis, customer service, and problem-solving skills at XYZ Insurance Company. At ABC Insurance Company, handled over 2000 claims while maintaining a 98% accuracy rate on all claim payments. Successfully identified fraudulent activities that saved the company $50K per year.
Determined claims analyst with 10+ years of experience developing and implementing claims-processing policies. Expertise in insurance claim analysis, contract interpretation, dispute resolution and customer service. Seeking to leverage exceptional problem-solving skills to join ABC Insurance as a senior claims analyst, helping the company grow by providing accurate and timely services for clients.
Detail-oriented claims analyst with 5+ years of experience assessing and verifying insurance claims. Looking to join ABC Insurance as a Claims Analyst, where I can apply my keen eye for detail and passion for accuracy when investigating customer claims. In previous roles, saved company over $1 million in fraudulent payouts by identifying incorrect information on submitted documents.
2. Experience / Employment
In the experience/employment/work history section, you should provide details on your past roles. This section should be written in reverse chronological order, meaning the most recent job is listed first.
When writing this section, stick to bullet points for easy reading and comprehension. Make sure that each point contains detail about what you did as well as quantifiable results achieved from your work.
For example, instead of saying “Processed insurance claims,” you could say “Evaluated 10+ medical insurance claims per day according to policy guidelines; reduced processing time by 20% through efficient data entry techniques.”
To write effective bullet points, begin with a strong verb or adverb. Industry specific verbs to use are:
- Investigated
- Analyzed
- Resolved
- Processed
- Assessed
- Documented
- Reconciled
- Evaluated
- Managed
- Researched
- Negotiated
- Adjudicated
- Settled
- Reported
Other general verbs you can use are:
- Achieved
- Advised
- Compiled
- Coordinated
- Demonstrated
- Developed
- Expedited
- Facilitated
- Formulated
- Improved
- Introduced
- Mentored
- Optimized
- Participated
- Prepared
- Presented
- Reduced
- Reorganized
- Represented
- Revised
- Spearheaded
- Streamlined
- Structured
- Utilized
Below are some example bullet points:
- Structured and implemented a new claims process that improved accuracy of payments by 15%, while ensuring compliance with all legal and regulatory requirements.
- Optimized existing procedures to reduce the average turnaround time per claim from 10 days to 4, resulting in quicker resolution for over 500 customers monthly.
- Successfully managed a team of 5 Claims Analysts responsible for reviewing complex insurance documents and resolving disputes within 48 hours on average each month; reduced customer complaints by 25%.
- Reported discrepancies between healthcare policies and actual payments accurately, enabling proper reimbursement rates across different providers within an 8-state region; saved $50K annually from fraudulent activities identified through audits & investigations conducted quarterly.
- Negotiated settlements with medical facilities as needed to resolve disputed claims promptly, maintaining an 85% success rate in successful resolutions without involving external mediation services or court proceedings.
- Revised over 300 insurance claims per month and successfully negotiated settlements with claimants, resulting in a 20% increase in savings for the company within the last year.
- Demonstrated expertise in interpreting complex legal documents to ensure that all claims were compliant with state regulations and industry standards; lowered errors by 10%.
- Utilized specialized software systems such as ClaimVantage and Verisk Analytics to track cases, analyze data points and generate detailed reports on claim statuses.
- Introduced process improvements which streamlined workflow processes from 72 hours to 48 hours average turnaround time on property damage claims; improved customer satisfaction rating by 25%.
- Thoroughly investigated suspicious or fraudulent activities related to submitted insurance applications or processed claims; identified $45,000 worth of frauds over the past 18 months through close examination of payee statements & policy details.
- Adjudicated over 250 insurance claims valued at over $2 million, ensuring accuracy and compliance with applicable regulations.
- Resolved customer disputes in a timely manner; reduced claim resolution time by 15%.
- Actively investigated suspicious or fraudulent claims to identify errors and discrepancies to minimize payouts for false/inaccurate information provided by customers.
- Settled complex high-value cases within minutes of negotiation, helping the company save an approximate $500K in potential losses per annum due to erroneous processing fees & inaccurate documentation issues reported by claimants.
- Facilitated accurate data entry into the internal system while providing top-notch customer service throughout each step of the process; improved overall complaint ratings from clients by 25% year-on-year.
- Represented an insurance company’s claims department, handling an average of 70+ client cases and resolving disputes within a timely manner.
- Processed over 500 validations for liability coverage, personal injury protection and medical payments; achieved 98% accuracy rate in verification process.
- Spearheaded investigations into all disputed claims to determine validity and ensured that appropriate actions were taken as per the policy guidelines; reduced resolution time by 25%.
- Competently managed high-profile cases involving bodily injury or property damage, successfully negotiating settlements with clients while ensuring compliance regulations were followed at all times.
- Formulated comprehensive reports summarizing the findings of each case and provided accurate documentation to support evidence; raised data entry efficiency by 40%.
- Analyzed and processed over 1,000 claims daily in a fast-paced insurance environment; identified and resolved discrepancies to reduce processing errors by 25%.
- Reconciled accounts using various methods of reconciliation such as P&L analysis, trial balances and trend tracking; improved accuracy rate from 65% to 95% within 6 months.
- Improved customer satisfaction ratings through timely resolution of disputes arising from claims payments & policy changes with minimal supervision required.
- Independently managed the end-to-end process for 100+ complex cases focusing on fraud prevention and risk mitigation strategies; reduced fraudulent activity by 30%.
- Coordinated closely with all stakeholders involved including customers, vendors, internal departments and external agencies to ensure proper closure of cases in compliance with industry regulations.
- Researched and analyzed medical records and insurance policies to determine the validity of claims, reducing claim discrepancy by 30% in a 3-month period.
- Participated in weekly meetings with members of other departments to discuss discrepancies between denied/approved claims and resolved issues within 24 hours on average.
- Resourcefully identified trends in fraudulent or suspicious activity while conducting reviews; reported 7 cases of fraud which resulted in a total savings of $25,000 for the company over 6 months.
- Expedited payments for valid claims by verifying accuracy and completeness prior to submission, increasing data entry efficiency by 10%.
- Documented all pertinent information regarding pending or approved/denied claims into an organized database system; successfully maintained 90+ files during each shift without any errors noted.
- Proficiently investigated 100+ insurance claims per day, ensuring that all data was accurate and up-to-date.
- Reduced fraudulent claims by 25% through detailed analysis of claim files and customer background checks; saved the company $10,000 in payroll costs over 6 months.
- Achieved a 98% accuracy rate when manually entering claim information into the computer system within 2 hours of receiving it from customers or agents; reduced average processing time for each case by 7 minutes.
- Analyzed historical medical records to determine whether treatments were medically necessary or not; identified 3 cases where patients received unnecessary services resulting in savings of $15,500 for the firm’s clients annually.
- Compiled weekly reports on new and existing cases for management review using statistical methods such as regression models to identify trends & patterns across different types of claims & policies.
3. Skills
Skill requirements will differ from employer to employer – this can easily be determined via the job advert. Organization ABC may be looking for someone with experience in medical claims while Organization XYZ may require a knowledge of auto insurance.
It is important to tailor the skills section of your resume according to each job you are applying for, as many employers utilize applicant tracking systems which scan resumes for certain keywords before passing them on to a human.
In addition to just listing relevant skills here, it’s also beneficial to discuss these further in other areas such as the summary or experience sections.
Below is a list of common skills & terms:
- Access
- Analysis
- Claim
- Claims Handling
- Claims Management
- Commercial Insurance
- Communication
- Customer Satisfaction
- Data Analysis
- Data Entry
- Employee Benefits
- Financial Analysis
- General Insurance
- HIPAA
- Health Insurance
- Healthcare
- Insurance
- Legal Liability
- Liability
- Medical Billing
- Medicare
- Process Improvement
- Property and Casualty Insurance
- Risk Management
- Social Networking
- Team Leadership
- Teamwork
- Time Management
- Underwriting
4. Education
Mentioning your education section on your resume is dependent on how far along you are in your career. If you just graduated and have no work experience, then include an education section below the objective statement. However, if you have years of experience as a claims analyst, it might be best to omit the education section altogether.
If including this information is necessary or desired, try to mention classes related to the claims analyst job duties that you applied for such as finance and accounting courses or legal studies.
Bachelor of Science in Business Administration
Educational Institution XYZ
Nov 2011
5. Certifications
Certifications demonstrate to potential employers that you have the knowledge and skills necessary for a particular job. It is important to include any certifications relevant to the position in your resume, as it will give hiring managers an indication of how well-versed you are in certain areas.
When listing out your certifications on your resume, be sure to include details such as when they were obtained and from which organization or institution. This will help demonstrate that these qualifications are up-to-date and valid.
Certified Professional Claims Analyst
Claims and Litigation Management Alliance (
May 2017
6. Contact Info
Your name should be the first thing a reader sees when viewing your resume, so ensure its positioning is prominent. Your phone number should be written in the most commonly used format in your country/city/state, and your email address should be professional.
You can also choose to include a link to your LinkedIn profile, personal website, or other online platforms relevant to your industry.
Finally, name your resume file appropriately to help hiring managers; for Abdiel Kautzer, this would be Abdiel-Kautzer-resume.pdf or Abdiel-Kautzer-resume.docx.
7. Cover Letter
Including a cover letter with your job application is a great way to make yourself stand out from the crowd. It should be made up of 2-4 paragraphs and provide additional information about you that isn’t already included in your resume.
Cover letters give employers an insight into who you are as a professional, what makes you unique, and why they should consider hiring you for the role. Although it’s not always necessary to include one, doing so can be beneficial when applying for jobs.
Below is an example cover letter:
Dear Edmund,
I am writing to apply for the Claims Analyst position at [company name]. I have a strong background in healthcare claims processing, as well as experience working with insurance companies and providers to resolve claims. In my previous role, I processed more than 1,000 claims per month and had a 98% accuracy rate. I also developed relationships with providers to ensure timely claim submission and follow-up on outstanding issues. My ability to work independently and take initiative will be an asset to your team.
In addition to my experience processing healthcare claims, I have strong analytical skills that would enable me to excel in this role. In my previous role, I utilized data analytics tools to identify errors in claim submissions and develop processes for preventing future errors. My analytical skills combined with my knowledge of the healthcare industry make me confident that I would be successful in this role.
I am excited about the opportunity to join [company name] as a Claims Analyst and contribute to your team’s success. Thank you for your time and consideration; I look forward to hearing from you soon.
Sincerely,
Abdiel
Claims Analyst Resume Templates
 Jerboa
Jerboa Fossa
Fossa Markhor
Markhor Cormorant
Cormorant Bonobo
Bonobo Dugong
Dugong Axolotl
Axolotl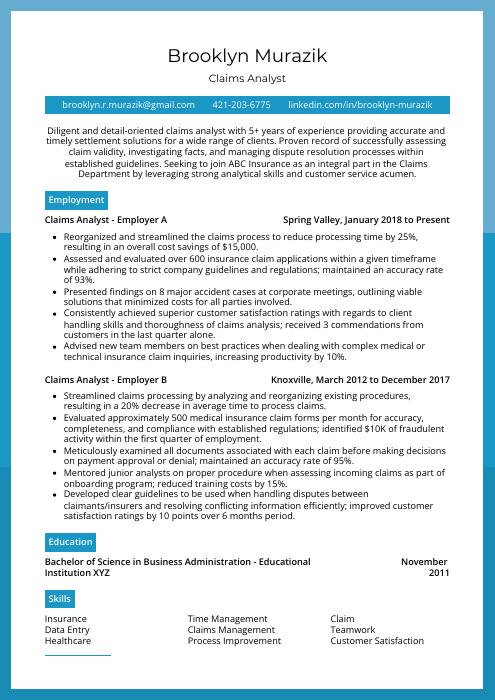 Rhea
Rhea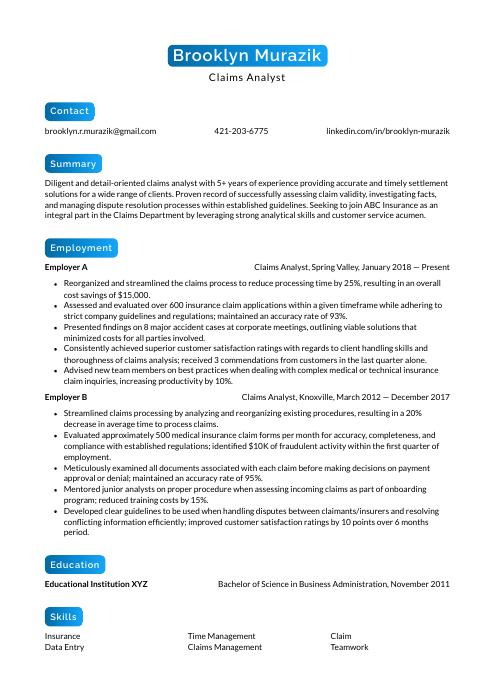 Kinkajou
Kinkajou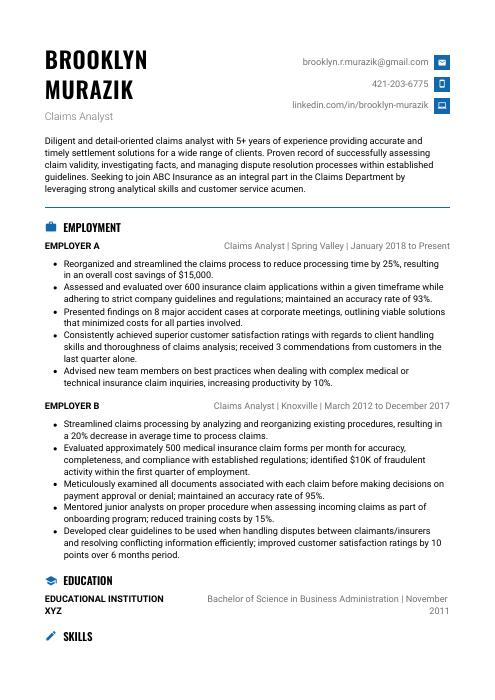 Echidna
Echidna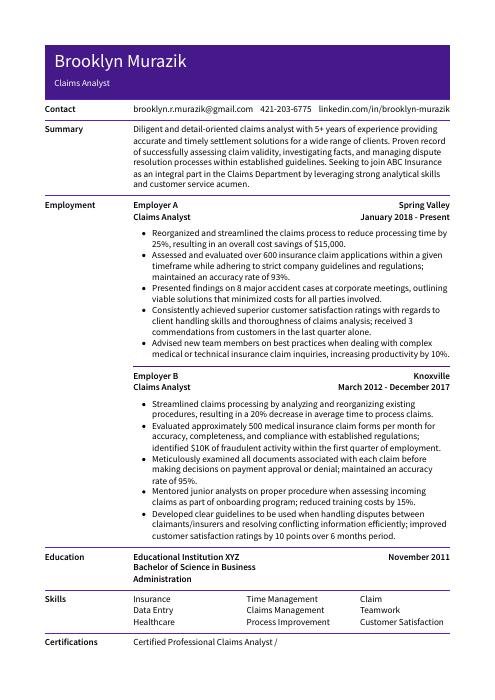 Pika
Pika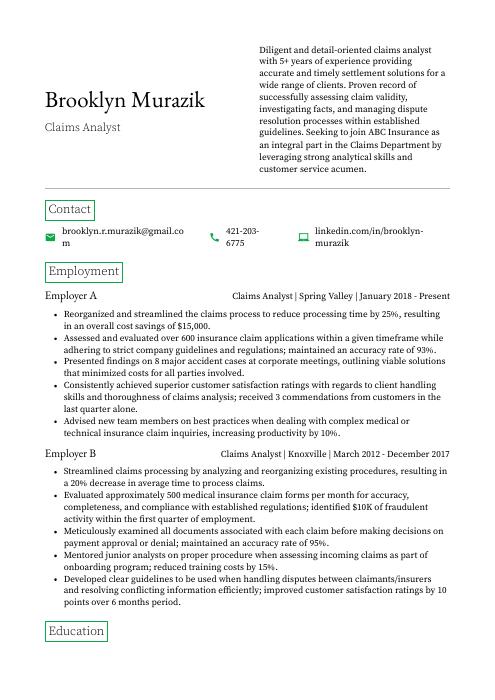 Quokka
Quokka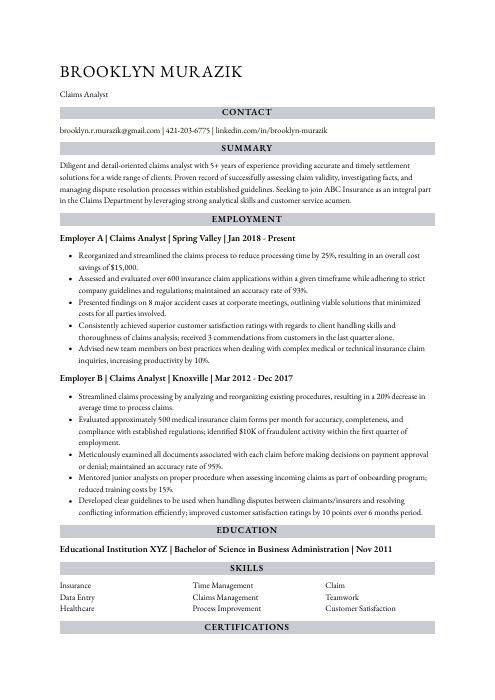 Numbat
Numbat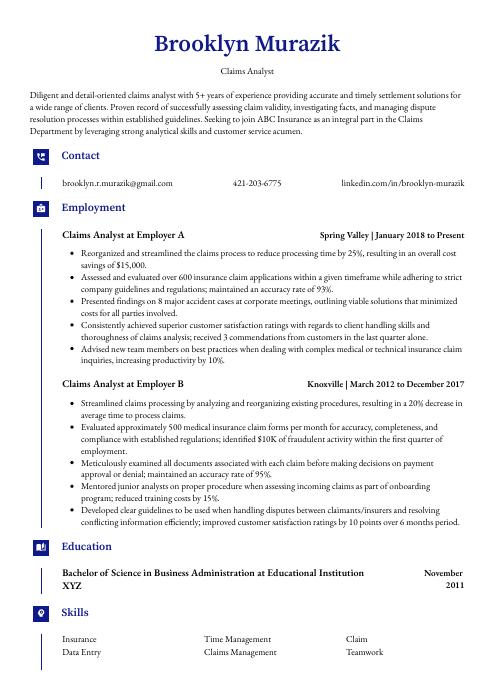 Gharial
Gharial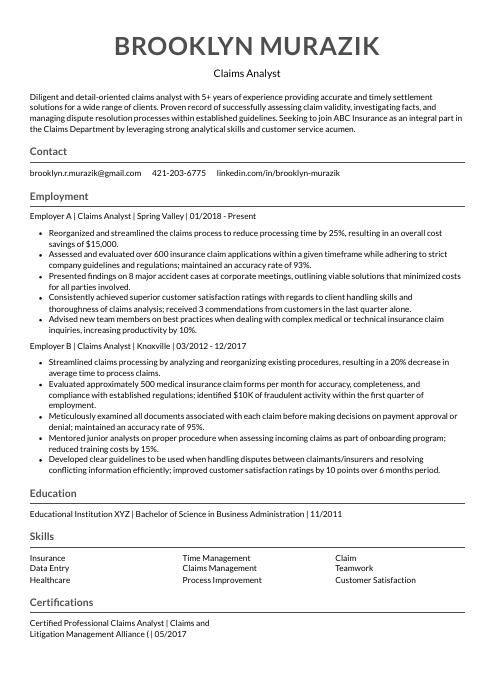 Indri
Indri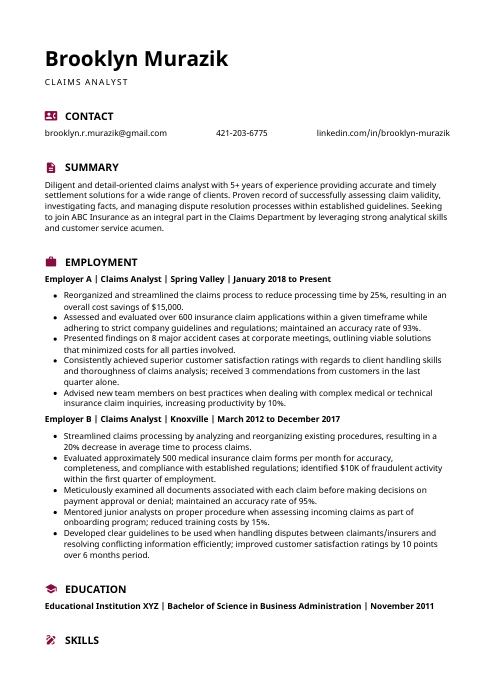 Hoopoe
Hoopoe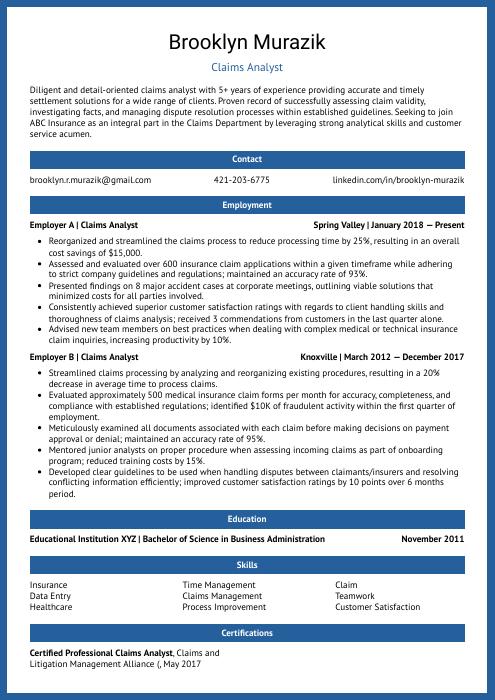 Ocelot
Ocelot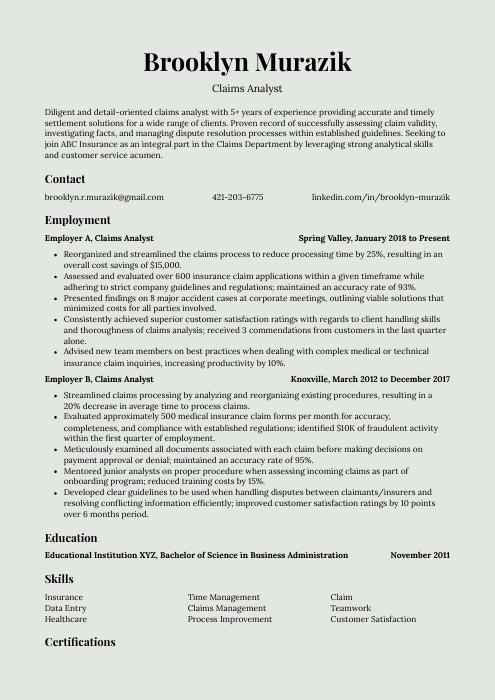 Saola
Saola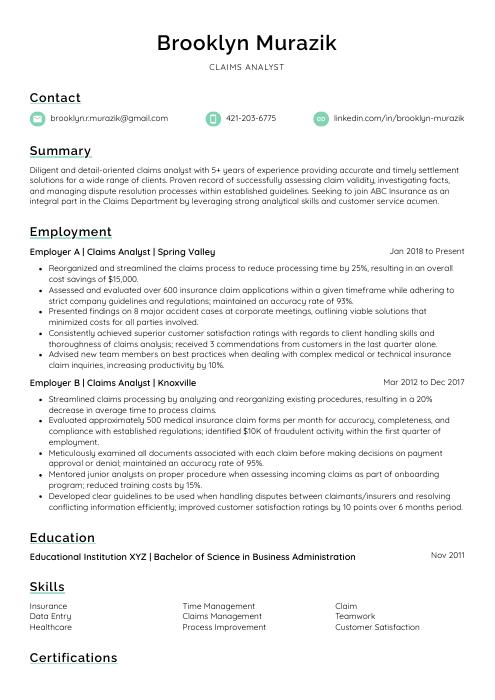 Lorikeet
Lorikeet Rezjumei
Rezjumei