Utilization Review Specialist Resume Guide
Utilization review specialists analyze medical records and health care data to assess the reasonableness, necessity, and appropriateness of services provided. They use their findings to make recommendations on whether or not a patient should be approved for treatment or procedures based on established criteria.
Your background in health care and insurance makes you an ideal candidate to fill the role of utilization review specialist. To get noticed by hiring managers, you must create a resume that showcases your qualifications and expertise.
This guide will walk you through the entire process of creating a top-notch resume. We first show you a complete example and then break down what each resume section should look like.
Table of Contents
The guide is divided into sections for your convenience. You can read it from beginning to end or use the table of contents below to jump to a specific part.
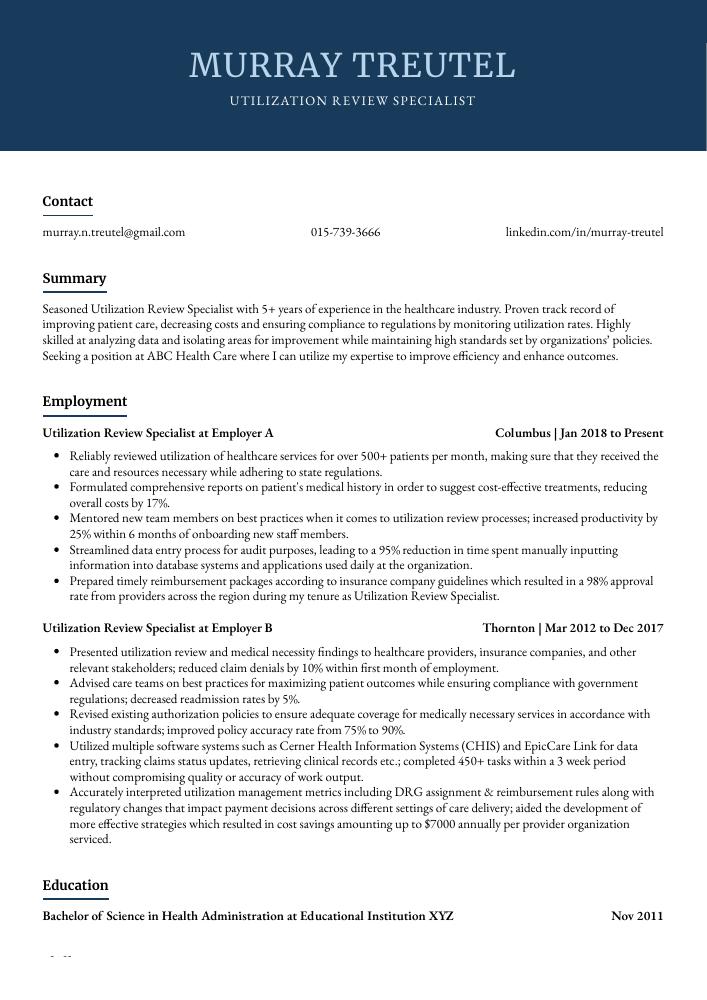
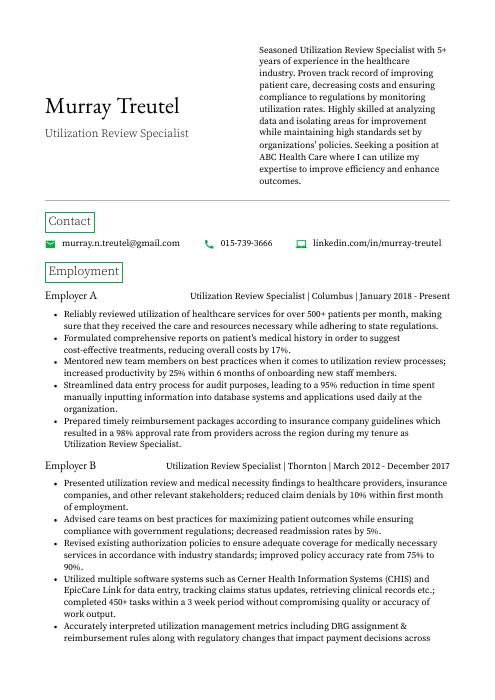
Utilization Review Specialist Resume Sample
Murray Treutel
Utilization Review Specialist
[email protected]
015-739-3666
linkedin.com/in/murray-treutel
Summary
Seasoned Utilization Review Specialist with 5+ years of experience in the healthcare industry. Proven track record of improving patient care, decreasing costs and ensuring compliance to regulations by monitoring utilization rates. Highly skilled at analyzing data and isolating areas for improvement while maintaining high standards set by organizations’ policies. Seeking a position at ABC Health Care where I can utilize my expertise to improve efficiency and enhance outcomes.
Experience
Utilization Review Specialist, Employer A
Columbus, Jan 2018 – Present
- Reliably reviewed utilization of healthcare services for over 500+ patients per month, making sure that they received the care and resources necessary while adhering to state regulations.
- Formulated comprehensive reports on patient’s medical history in order to suggest cost-effective treatments, reducing overall costs by 17%.
- Mentored new team members on best practices when it comes to utilization review processes; increased productivity by 25% within 6 months of onboarding new staff members.
- Streamlined data entry process for audit purposes, leading to a 95% reduction in time spent manually inputting information into database systems and applications used daily at the organization.
- Prepared timely reimbursement packages according to insurance company guidelines which resulted in a 98% approval rate from providers across the region during my tenure as Utilization Review Specialist.
Utilization Review Specialist, Employer B
Thornton, Mar 2012 – Dec 2017
- Presented utilization review and medical necessity findings to healthcare providers, insurance companies, and other relevant stakeholders; reduced claim denials by 10% within first month of employment.
- Advised care teams on best practices for maximizing patient outcomes while ensuring compliance with government regulations; decreased readmission rates by 5%.
- Revised existing authorization policies to ensure adequate coverage for medically necessary services in accordance with industry standards; improved policy accuracy rate from 75% to 90%.
- Utilized multiple software systems such as Cerner Health Information Systems (CHIS) and EpicCare Link for data entry, tracking claims status updates, retrieving clinical records etc.; completed 450+ tasks within a 3 week period without compromising quality or accuracy of work output.
- Accurately interpreted utilization management metrics including DRG assignment & reimbursement rules along with regulatory changes that impact payment decisions across different settings of care delivery; aided the development of more effective strategies which resulted in cost savings amounting up to $7000 annually per provider organization serviced.
Skills
- Medical Coding
- Clinical Documentation
- Health Insurance Policies
- Medical Terminology
- HIPAA Compliance
- Utilization Management
- Claims Processing
- Quality Assurance
- Data Analysis
Education
Bachelor of Science in Health Administration
Educational Institution XYZ
Nov 2011
Certifications
Certified Utilization Review Specialist (CURS)
American
May 2017
1. Summary / Objective
Your resume summary should provide a snapshot of your qualifications as a utilization review specialist. Include any relevant certifications, such as the Certified Utilization Review Professional (CURP) certification you recently earned, and mention how many years of experience in the field you have. You can also highlight any successful projects or initiatives that demonstrate your ability to manage complex cases and ensure compliance with regulations.
Below are some resume summary examples:
Passionate utilization review specialist with 8+ years of experience in healthcare quality management. Skilled at making quick decisions to ensure that care is appropriate, medically necessary and cost-effective for a variety of insurance payers such as Medicare, Medicaid and private insurers. Experienced in analyzing patient medical records for coding accuracy and compliance with regulatory guidelines. At XYZ Medical Center, reduced the number of denied claims by 30%.
Well-rounded utilization review specialist with 8+ years of experience in healthcare. Skilled at performing medical necessity reviews, coordinating pre-certification and concurrent utilization activities for large insurance companies. Proven track record of reducing costs by 10% while ensuring quality care delivery to patients. Experienced in developing effective strategies to improve operational efficiency without compromising patient safety or satisfaction levels.
Committed utilization review specialist with 8+ years of experience in healthcare and managed care. At XYZ, identified potential opportunities for cost savings while ensuring compliance with all applicable laws and regulations. Demonstrated proficiency in using data to identify trends in utilization and quality of services provided by providers. Skilled at working collaboratively with stakeholders from payers, providers, members, patients’ families and employers.
Diligent Utilization Review Specialist with 5+ years of experience in healthcare and insurance industry. Adept at evaluating patient medical records to ensure cost-effective care, compliant with standards set by government regulations. Proven success in reducing costs for a major managed care organization while maintaining quality of service. Seeking opportunity to apply knowledge and expertise as Utilization Review Specialist at ABC Healthcare Services.
Proficient Utilization Review Specialist with 5+ years of experience in ensuring quality and compliance standards are met. Experienced in providing medical necessity reviews on a variety of services, such as hospitalizations, physician visits, home health care services and durable medical equipment requests. Skilled at working effectively with physicians to ensure timely service delivery while maintaining cost-effective utilization practices.
Determined utilization review specialist with 5+ years of experience in performing utilization reviews and analyzing data to ensure optimal patient care. At XYZ, conducted over 200 concurrent and retrospective authorization requests for the hospital’s mental health services. Recognized by peers as a team-oriented individual who is detail oriented while remaining focused on cost containment strategies that maintain quality of care standards.
Skilled utilization review specialist with 6+ years of experience in reviewing and approving medical care services for insurance companies. Adept at interpreting complex regulations, developing utilization plans, and managing authorization processes. At Company X, reduced turnaround times by 10% while ensuring quality standards were met or exceeded. Seeking to use my expertise to help ABC achieve its objectives.
Driven Utilization Review Specialist with 5+ years of experience in healthcare and managed care. Seeking to join ABC Healthcare as the new Utilization Review Specialist and leverage expertise in pre-authorizations, utilization management, discharge planning, and quality improvement initiatives. At XYZ Inc., reduced denials by 15% via utilizing data analysis tools for monitoring utilization trends.
2. Experience / Employment
Next comes the work history section. This should be written in reverse chronological order, with the most recent job listed first.
When writing this section, stick to bullet points and provide detail on what you did and the results achieved. For example, instead of saying “Reviewed medical records,” you could say “Evaluated patient medical records for accuracy and completeness according to established standards; identified errors or omissions that led to a 5% reduction in denials.”.
You also want to include any awards or recognition received while working in each role. Doing so can help demonstrate your accomplishments more clearly.
To write effective bullet points, begin with a strong verb or adverb. Industry specific verbs to use are:
- Evaluated
- Assessed
- Analyzed
- Monitored
- Documented
- Researched
- Interpreted
- Coordinated
- Reported
- Reviewed
- Audited
- Reconciled
- Processed
- Resolved
Other general verbs you can use are:
- Achieved
- Advised
- Compiled
- Demonstrated
- Developed
- Expedited
- Facilitated
- Formulated
- Improved
- Introduced
- Mentored
- Optimized
- Participated
- Prepared
- Presented
- Reduced
- Reorganized
- Represented
- Revised
- Spearheaded
- Streamlined
- Structured
- Utilized
Below are some example bullet points:
- Structured utilization review processes for over 20 hospitals, reducing denials by 30% and increasing first-time claim approval rate to 95%.
- Reported utilization trends and issues to stakeholders while recommending changes in order to meet established performance goals; cut overall healthcare costs by $200K within 6 months.
- Improved the accuracy of medical claims through managing data entry personnel and verifying entered information with patient records; reduced errors from 17% to 3%.
- Reconciled discrepancies between billing department/payer information & provider’s clinical documentation as needed, ensuring timely reimbursement collection without any delay.
- Proficiently managed authorizations for services such as radiology, laboratory tests and hospital stays according to insurance plan guidelines; achieved 100% compliance with state regulations governing Utilization Review activities within one year of employment.
- Resolved and processed over 2000 utilization reviews in a timely manner, ensuring that medical treatments and services adhered to insurance company standards while decreasing turnaround time by 25%.
- Documented detailed reports on all completed utilization reviews, outlining reasons for approval or denial; reduced administrative errors by 30% through careful inspection of patient records.
- Optimized the overall process of utilization review with innovative strategies such as designing new forms and creating collaborative workflows between departments; improved efficiency by 40%.
- Compiled comprehensive monthly summaries of all approved/denied cases using data from multiple sources; identified discrepancies in procedures which led to $10,000 savings per quarter throughout the organization.
- Diligently monitored changes in healthcare regulations & guidelines related to utilization review processes to ensure compliance with local laws and increase accuracy rates across the board by 10%.
- Achieved 98% accuracy in reviewing and approving insurance claims, ensuring that all healthcare providers were appropriately reimbursed within 5 days of initial submission.
- Resourcefully identified medical errors or discrepancies on patient records to prevent potential fraud cases; saved the company $30K over 6 months with improved utilization review procedures.
- Facilitated successful communication between patients, health plan members and healthcare facilities regarding billing inquiries & other related issues; reduced customer complaints by 45%.
- Processed 2,500+ authorization requests per month for medical services such as home health care visits, hospitalizations and outpatient treatments following established protocols & guidelines set forth by regulatory bodies like CMS/Medicare Medicaid etc..
- Demonstrated expertise in using different computer programs including MS Office Suite (Excel), Epic EHR software and CPT coding manuals to ensure accurate documentation of patient information & reimbursement processes at all times.
- Audited and processed 500+ patient medical records and utilization reviews per month, ensuring accuracy of billing codes, authorization requests and review outcomes.
- Expedited the implementation of new strategies for managing utilization trends to reduce healthcare costs by 10% in 6 months.
- Coordinated with insurance companies to ensure compliance with coverage requirements; successfully resolved 120+ disputes related to reimbursement claims within a 3-month period.
- Successfully improved turnaround time on account denials from 5 days to 2 days through streamlined processes and effective communication skills across all departments involved in the process chain flow management system (PCFMS).
- Reorganized over 1,000 files containing prior authorizations/denials data into an organized electronic filing system that increased efficiency by 25%.
- Analyzed medical records and claims data to accurately assess the utilization of healthcare services, resulting in a 10% decrease in unnecessary costs.
- Monitored health plan members’ care utilization patterns for any potential misuse or underuse of medical treatments; identified $20,000 worth of fraudulent activities over 3 months.
- Reviewed up to 400 patient files per week on an independent basis with attention to detail and accuracy; reduced turnaround time by 15%.
- Independently managed all aspects of clinical review processes while meeting strict regulatory guidelines & deadlines set by insurers & government agencies such as Medicaid & Medicare programs.
- Researched best practices related to current evidence-based standards regarding chronic condition management, preventive medicine protocols and quality improvement initiatives for optimal outcomes at minimum cost savings annually.
- Confidently evaluated and analyzed medical records of 250+ patients per week to determine the appropriateness, necessity and quality of care provided in accordance with policy guidelines; reduced overall healthcare costs by 10%.
- Introduced best practices for utilization review process into practice that enabled faster data collection & decision making while maintaining accuracy; increased efficiency by 8 hours a day.
- Developed reports on utilization patterns, trends and opportunities for improvement based on audit findings; identified cost savings opportunities totaling $100K in the first year alone.
- Interpreted complex clinical information from multiple sources such as patient charts, lab results & physician notes quickly and accurately to ensure optimal health outcomes without sacrificing safety or quality standards.
- Successfully collaborated with other members of multidisciplinary teams including physicians, nurses & administrators to clarify diagnosis codes or procedures whenever needed during reviews.
- Assessed health care services of over 400 patients per month, ensuring compliance with all regulations and that insurance coverage was maximized.
- Effectively communicated utilization review decisions to medical providers via phone, email and written correspondence; reduced appeals by 30%.
- Spearheaded the development of a new methodology for evaluating patient health needs; increased cost savings by $25K annually.
- Participated in weekly meetings with other professionals to discuss difficult cases and formulate solutions to meet patient needs without compromising quality standards or exceeding budget constraints.
- Represented the organization at regional conferences related to utilization management initiatives, collaborating with industry leaders on best practices for promoting improved outcomes & system efficiencies across healthcare organizations.
3. Skills
Even though two organizations are hiring for the same role, the skillset they want an ideal candidate to possess could differ significantly. For instance, one may be on the lookout for an individual who is knowledgeable about Medicare and Medicaid regulations, while the other may be looking for someone who has experience with insurance claims processing.
This means that you should customize your skills section to each job posting; this will increase the likelihood of getting noticed by an employer’s applicant tracking system (ATS). An ATS scans resumes for certain keywords before passing them on to a human recruiter or hiring manager.
In addition to listing relevant qualifications in this section, you should also discuss some of these qualities in more detail elsewhere on your resume – such as within the summary statement or work history sections.
Below is a list of common skills & terms:
- Claims Processing
- Clinical Documentation
- Data Analysis
- HIPAA Compliance
- Health Insurance Policies
- Interpersonal Communication
- Medical Coding
- Medical Terminology
- Quality Assurance
- Utilization Management
4. Education
Mentioning an education section on your resume will depend on how much experience you have in the field. If you just graduated and don’t have any prior work experience, it is important to include an education section below your objective statement. However, if you already have years of utilization review specialist experience under your belt, including this information may not be necessary.
If an education section is included, make sure to mention relevant courses or subjects related to the utilization review specialist role that demonstrate what skills and knowledge you possess.
Bachelor of Science in Health Administration
Educational Institution XYZ
Nov 2011
5. Certifications
Certifications demonstrate to potential employers that you have a certain level of expertise in the field. They are also an indication that you have taken the time and effort to stay up-to-date with industry trends, as well as having invested in your professional development.
If there is a certification relevant to the job role for which you are applying, make sure it is included on your resume so hiring managers can see how qualified and experienced you are.
Certified Utilization Review Specialist (CURS)
American
May 2017
6. Contact Info
Your name should be the first thing a reader sees when viewing your resume, so ensure its positioning is prominent. Your phone number should be written in the most commonly used format in your country/city/state, and your email address should be professional.
You can also choose to include a link to your LinkedIn profile, personal website, or other online platforms relevant to your industry.
Finally, name your resume file appropriately to help hiring managers; for Murray Treutel, this would be Murray-Treutel-resume.pdf or Murray-Treutel-resume.docx.
7. Cover Letter
Including a cover letter in your job application is a great way to provide the hiring manager with more information about yourself. It usually consists of 2-4 paragraphs and offers you an opportunity to explain why you are the ideal candidate for that particular position.
Although not every employer requires a cover letter, it can be beneficial in demonstrating your enthusiasm for the role as well as highlighting some key skills or experiences which cannot be found on your resume alone. Writing one will help make sure that you stand out from the competition!
Below is an example cover letter:
Dear Kevin,
I am writing to apply for the Utilization Review Specialist position at XYZ Company. As a highly skilled and experienced utilization review specialist with more than 10 years of experience working in the healthcare industry, I am confident that I would be a valuable asset to your team.
In my current role as Utilization Review Specialist at ABC Corporation, I am responsible for conducting reviews of patient medical records to ensure that the care they received was appropriate and necessary. In addition, I make recommendations for discharge planning and post-discharge follow-up care. Through my work, I have developed strong analytical and problem-solving skills that I believe would benefit your organization.
I have also gained extensive experience dealing with insurance companies and other third-party payers. In many cases, these organizations are reluctant to approve coverage for certain types of care; however, through my persistence and negotiation skills, I have been successful in securing approval in a majority of cases. This has resulted in significant savings for my employer while also ensuring that patients receive the care they need.
If given the opportunity, I am confident that I can provide similar results for XYZ Company. Thank you for your time and consideration; please do not hesitate to contact me if you have any questions about my qualifications or suitability for this position.
Sincerely,
Murray
Utilization Review Specialist Resume Templates
 Quokka
Quokka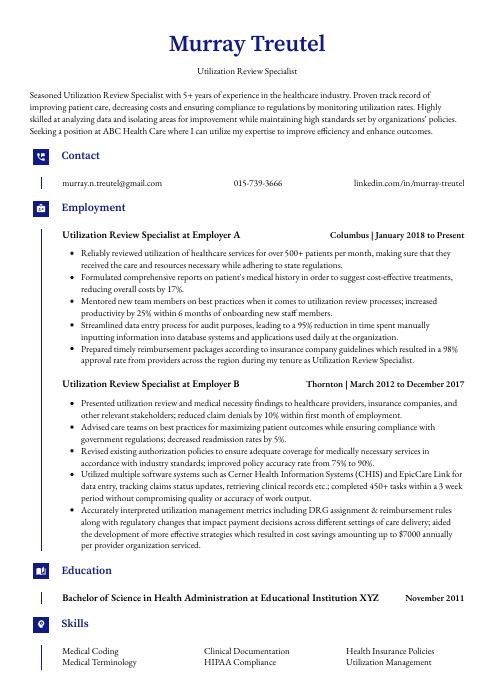 Gharial
Gharial Numbat
Numbat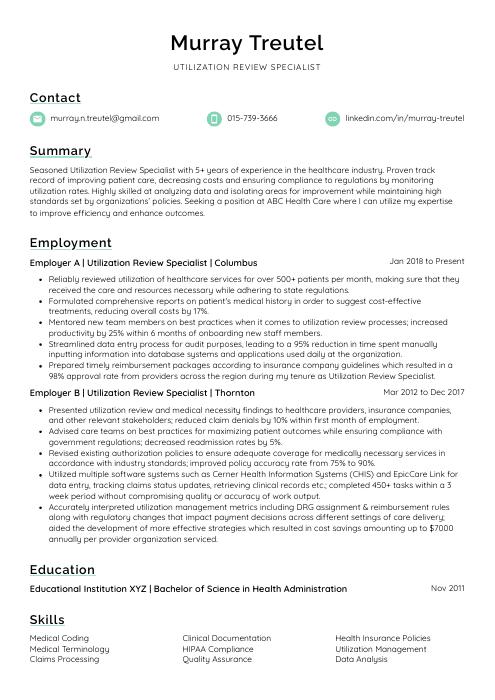 Lorikeet
Lorikeet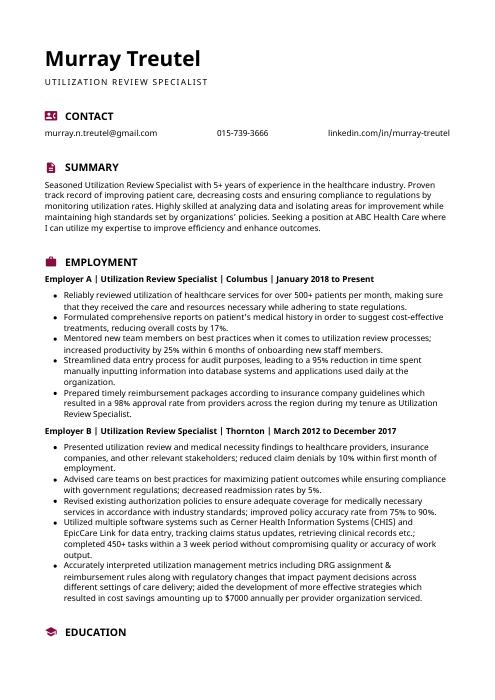 Hoopoe
Hoopoe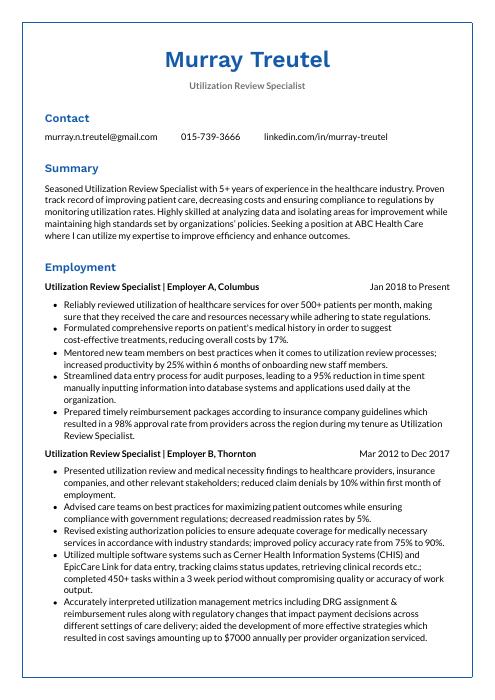 Markhor
Markhor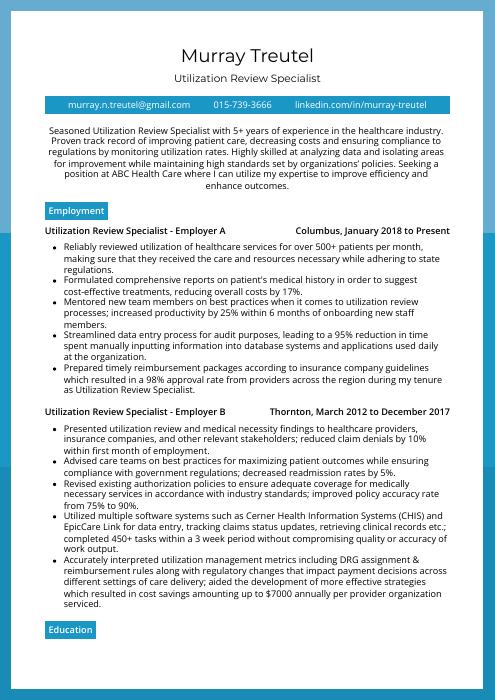 Rhea
Rhea Saola
Saola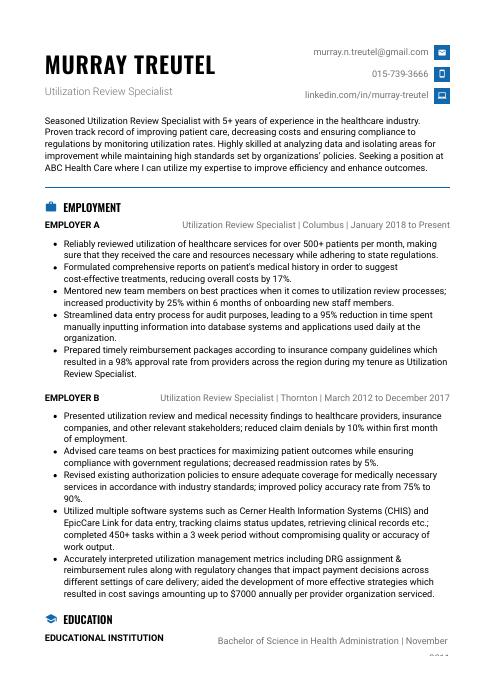 Echidna
Echidna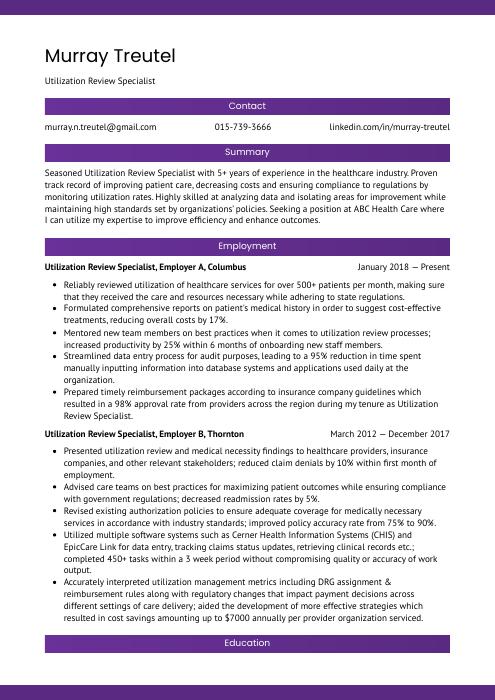 Jerboa
Jerboa Dugong
Dugong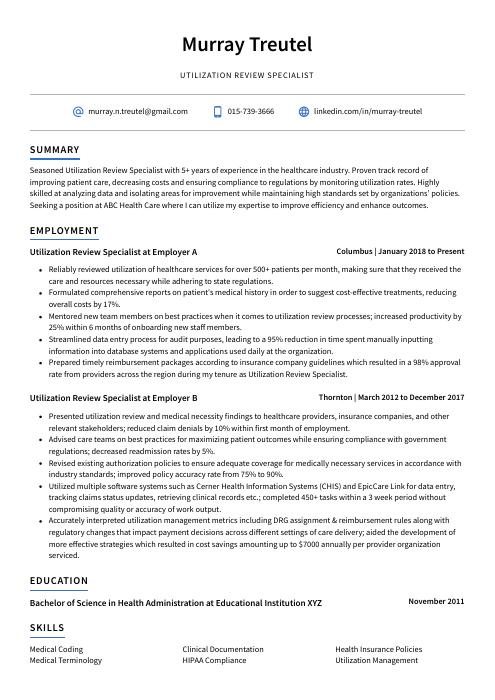 Axolotl
Axolotl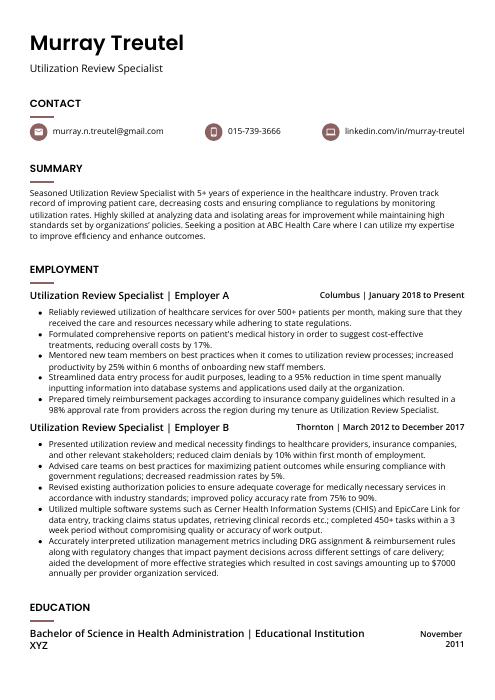 Fossa
Fossa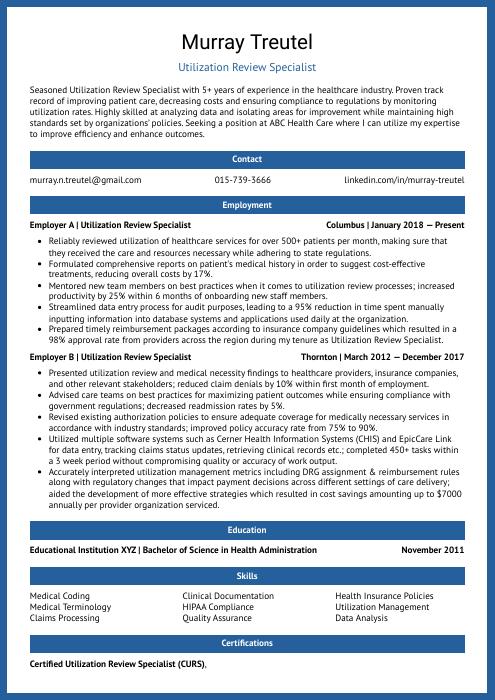 Ocelot
Ocelot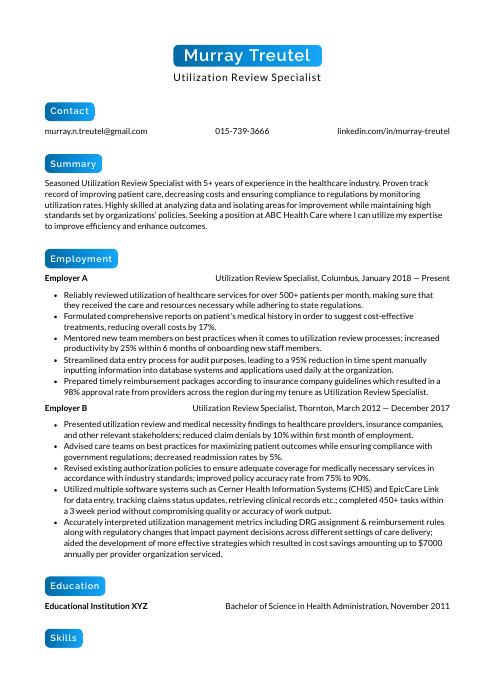 Kinkajou
Kinkajou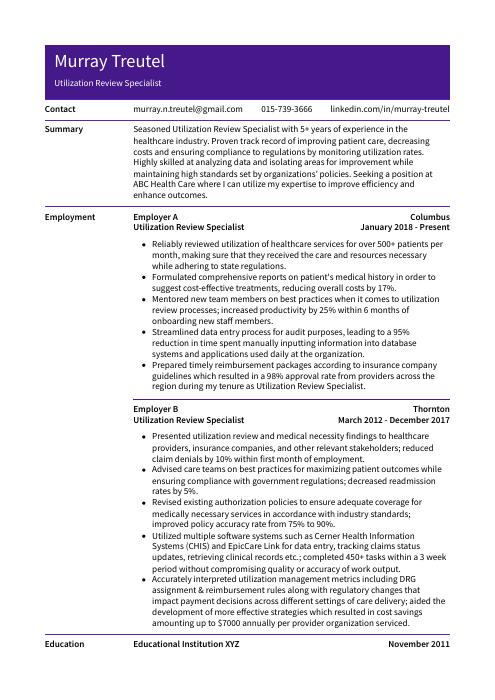 Pika
Pika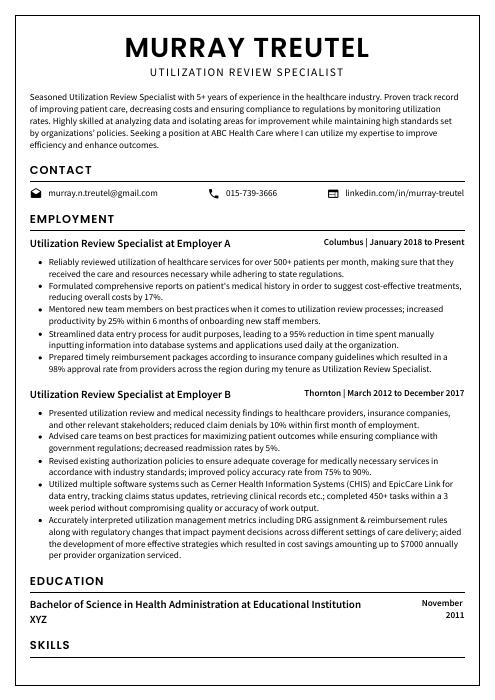 Cormorant
Cormorant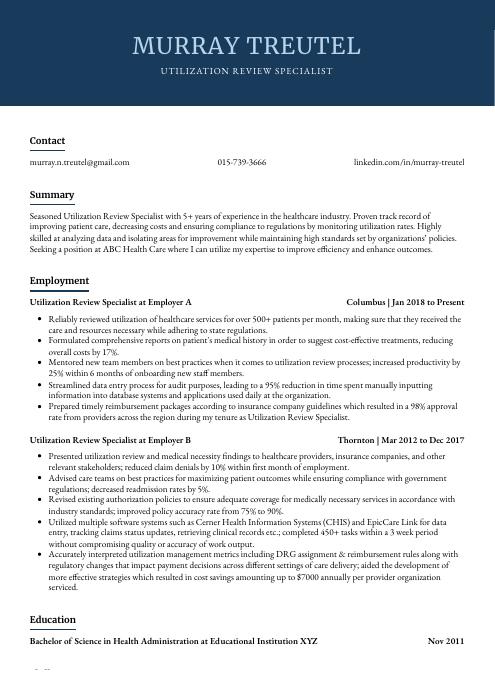 Bonobo
Bonobo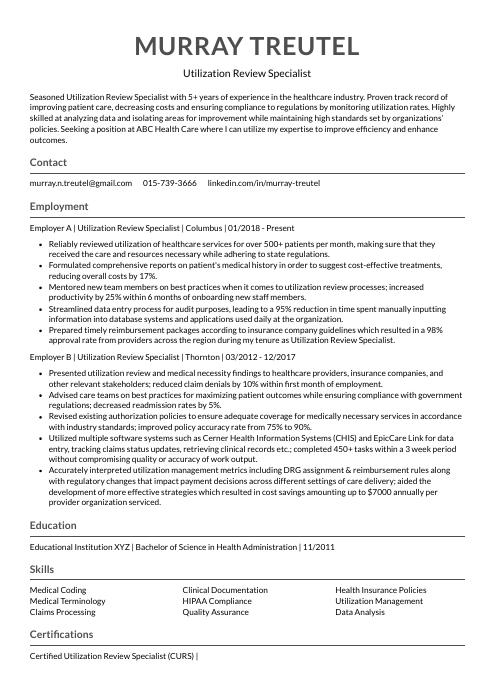 Indri
Indri Rezjumei
Rezjumei