Revenue Integrity Analyst Resume Guide
Revenue integrity analysts are responsible for ensuring the accuracy and completeness of revenue data. They review financial information, analyze trends, identify discrepancies or errors in revenue reporting systems and processes, and develop plans to rectify any issues that arise. Additionally, they monitor compliance with organizational policies related to billing practices as well as government regulations.
You are a true asset to any healthcare facility, with your ability to uncover billing and coding errors. But potential employers don’t know who you are yet, so you must write an impressive resume that presents your talents.
This guide will walk you through the entire process of creating a top-notch resume. We first show you a complete example and then break down what each resume section should look like.
Table of Contents
The guide is divided into sections for your convenience. You can read it from beginning to end or use the table of contents below to jump to a specific part.
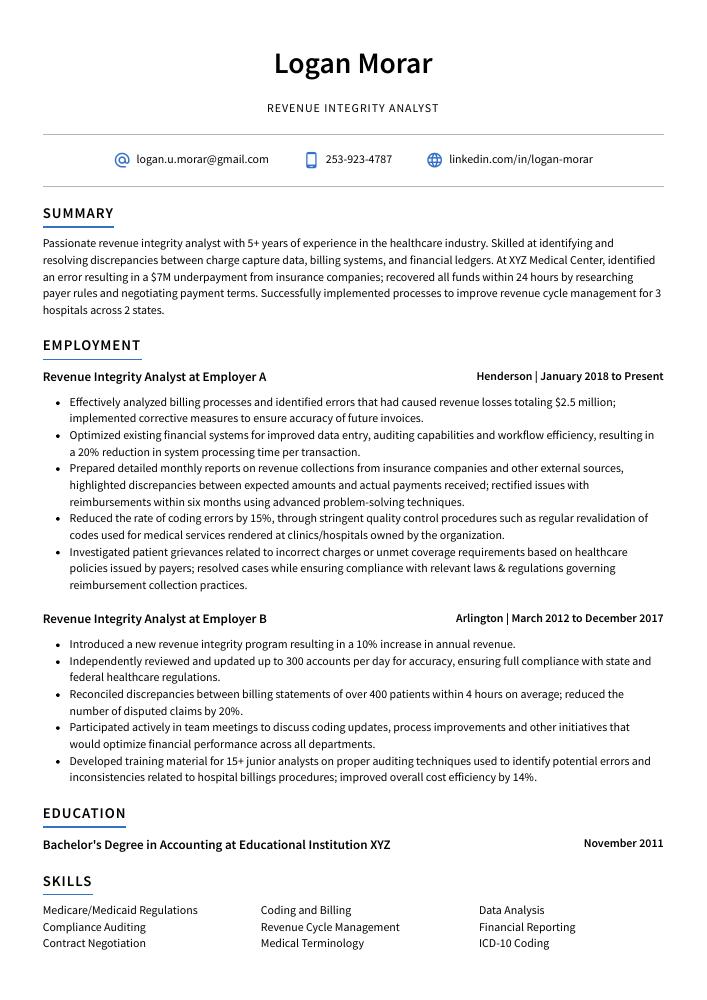
Revenue Integrity Analyst Resume Sample
Logan Morar
Revenue Integrity Analyst
[email protected]
253-923-4787
linkedin.com/in/logan-morar
Summary
Passionate revenue integrity analyst with 5+ years of experience in the healthcare industry. Skilled at identifying and resolving discrepancies between charge capture data, billing systems, and financial ledgers. At XYZ Medical Center, identified an error resulting in a $7M underpayment from insurance companies; recovered all funds within 24 hours by researching payer rules and negotiating payment terms. Successfully implemented processes to improve revenue cycle management for 3 hospitals across 2 states.
Experience
Revenue Integrity Analyst, Employer A
Henderson, Jan 2018 – Present
- Effectively analyzed billing processes and identified errors that had caused revenue losses totaling $2.5 million; implemented corrective measures to ensure accuracy of future invoices.
- Optimized existing financial systems for improved data entry, auditing capabilities and workflow efficiency, resulting in a 20% reduction in system processing time per transaction.
- Prepared detailed monthly reports on revenue collections from insurance companies and other external sources, highlighted discrepancies between expected amounts and actual payments received; rectified issues with reimbursements within six months using advanced problem-solving techniques.
- Reduced the rate of coding errors by 15%, through stringent quality control procedures such as regular revalidation of codes used for medical services rendered at clinics/hospitals owned by the organization.
- Investigated patient grievances related to incorrect charges or unmet coverage requirements based on healthcare policies issued by payers; resolved cases while ensuring compliance with relevant laws & regulations governing reimbursement collection practices.
Revenue Integrity Analyst, Employer B
Arlington, Mar 2012 – Dec 2017
- Introduced a new revenue integrity program resulting in a 10% increase in annual revenue.
- Independently reviewed and updated up to 300 accounts per day for accuracy, ensuring full compliance with state and federal healthcare regulations.
- Reconciled discrepancies between billing statements of over 400 patients within 4 hours on average; reduced the number of disputed claims by 20%.
- Participated actively in team meetings to discuss coding updates, process improvements and other initiatives that would optimize financial performance across all departments.
- Developed training material for 15+ junior analysts on proper auditing techniques used to identify potential errors and inconsistencies related to hospital billings procedures; improved overall cost efficiency by 14%.
Skills
- Medicare/Medicaid Regulations
- Coding and Billing
- Data Analysis
- Compliance Auditing
- Revenue Cycle Management
- Financial Reporting
- Contract Negotiation
- Medical Terminology
- ICD-10 Coding
Education
Bachelor’s Degree in Accounting
Educational Institution XYZ
Nov 2011
Certifications
Certified Revenue Integrity Analyst
American Association of Professional Coders
May 2017
1. Summary / Objective
Your resume summary is the first thing a potential employer will read, so make sure it grabs their attention. As a revenue integrity analyst, you can use your summary to highlight key skills such as data analysis and financial auditing experience. You could also mention any certifications or awards you have received in this field, as well as how many years of experience you have working with healthcare organizations.
Below are some resume summary examples:
Proficient Revenue Integrity Analyst with 6+ years of experience in the healthcare industry. Seeking to leverage expertise and knowledge of coding, billing compliance, and medical terminology to maximize revenue at XYZ. At ABC Company, identified $1.2M in underpayments by analyzing complex claims data sets and developing best practices for accurate payment processing. Proven ability to build strong relationships with internal stakeholders as well as external vendors/payers for improved audit outcomes.
Talented revenue integrity analyst with 3+ years of experience ensuring compliance and accuracy in financial operations. Accomplished at interpreting complex regulations and providing insights to optimize the revenue cycle for healthcare organizations. Seeking to join ABC Healthcare as a Revenue Integrity Analyst, leveraging strong communication skills, attention to detail, and problem-solving abilities to identify discrepancies in billing processes while minimizing risk exposure.
Seasoned revenue integrity analyst with 5+ years of experience in healthcare billing and coding. Expertise in auditing and managing accounts receivable for various organizations to ensure accuracy, compliance, and proper reimbursement. At XYZ, identified a discrepancy resulting in $200K savings per month through improved revenue cycle management processes. Strong analytical skills combined with excellent communication abilities make me an ideal candidate for this role.
Energetic and detail-oriented revenue integrity analyst with 5+ years of experience in healthcare billing and reimbursement. Skilled at identifying and recovering lost payments, reducing backlogs, ensuring accurate claim coding, improving accounts receivable cycles, and increasing profitability for clients. Seeking to join ABC Healthcare as a Revenue Integrity Analyst to utilize my expertise in driving process improvements that result in increased revenue generation.
Hard-working revenue integrity analyst with 7+ years of experience in healthcare revenue cycle management. Expertise in identifying potential risks and mitigating financial losses on the accounts receivable side to ensure accuracy of patient billing data. At XYZ, reduced annual AR write-off by 30% through diligent analysis and proactive problem solving. Seeking to join ABC Company as a Revenue Integrity Analyst for continued success and growth.
Well-rounded revenue integrity analyst with 5+ years of experience overseeing financial operations for hospitals and healthcare organizations. Experienced in conducting data analysis, developing rate structures, preparing reports on revenue trends, and improving billing processes to ensure compliance with regulatory laws. Seeking an opportunity at ABC Health Systems where I can apply my expertise to strengthen the organization’s fiscal health.
Amicable revenue integrity analyst with a passion for accuracy and compliance. 5+ years of experience auditing, reconciling, validating and analyzing data to ensure billing accuracy. Contributed to $1M in annual savings by identifying and correcting coding errors that resulted from insufficient training practices. Seeking an opportunity at ABC Healthcare Solutions where I can apply my knowledge towards optimizing reimbursement processes.
Accomplished Revenue Integrity Analyst with 8+ years of experience in the healthcare industry. Experienced in auditing, researching and analyzing claims/billing data for accuracy and compliance as well as developing strategies to enhance revenue integrity. Highly organized individual with excellent problem-solving skills. Interacted professionally with all levels of personnel within an organization from medical staff to executives.
2. Experience / Employment
The employment (or experience) section is where you provide details on your work history. This should be written in reverse chronological order, with the most recent job listed first.
When stating what you did at each role, stick to bullet points as much as possible. Doing so allows the reader to quickly digest what you have to say without getting bogged down in too many details. You want to take some time and think about how best to explain your duties and accomplishments using quantifiable results whenever possible.
For example, instead of saying “Audited hospital accounts,” you could say, “Performed comprehensive audits of over 300 hospital accounts per month resulting in a 10% increase in reimbursement accuracy.”
To write effective bullet points, begin with a strong verb or adverb. Industry specific verbs to use are:
- Analyzed
- Monitored
- Investigated
- Reconciled
- Resolved
- Documented
- Reported
- Identified
- Assessed
- Evaluated
- Collaborated
- Developed
- Implemented
- Optimized
Other general verbs you can use are:
- Achieved
- Advised
- Compiled
- Coordinated
- Demonstrated
- Expedited
- Facilitated
- Formulated
- Improved
- Introduced
- Mentored
- Participated
- Prepared
- Presented
- Reduced
- Reorganized
- Represented
- Revised
- Spearheaded
- Streamlined
- Structured
- Utilized
Below are some example bullet points:
- Diligently identified and corrected errors in billing codes, fee schedules, contractual allowances and other revenue-related sources for over 200 clients; resulted in a reduction of $2 million worth of incorrect charges.
- Facilitated the review of patient claims to ensure compliance with applicable regulations; increased accuracy rate from 80% to 95%.
- Achieved a 20% increase in reimbursement rates by accurately coding treatments and procedures according to current guidelines on state/federal health insurance programs.
- Identified discrepancies between charge data collected from multiple departments across the organization; developed new strategies to improve consistency throughout all processes for greater efficiency & cost savings (saved an average of 8 hours per week).
- Compiled comprehensive reports detailing audit findings based on analysis of financial records such as invoices, statements and contract documents while ensuring that HIPAA privacy rules were followed at all times.
- Implemented new policies and procedures to improve revenue integrity accuracy, resulting in an 18% increase of accurate account coding.
- Competently identified billing discrepancies and errors within the system; successfully resolved 95% of them with minimal financial impact on the organization.
- Resolved reimbursement issues by analyzing payment discrepancies between payer contracts and actual amount billed for services rendered; reclaimed $100,000+ lost revenues for the company.
- Reported all findings from audits involving Medicare/Medicaid payments, insurance claims processing activities and other related topics directly to upper management promptly upon completion of audit reviews.
- Streamlined manual processes by creating automated tools utilizing Microsoft Excel VBA language which increased efficiency levels by 10%.
- Analyzed billing trends and claims data for over 500 healthcare providers to identify areas of revenue leakage, resulting in a 12% increase in total annual collections.
- Mentored junior analysts on the use of medical coding systems and best practices when conducting root cause analysis; increased accuracy by 25%.
- Resourcefully identified billing discrepancies across multiple payer contracts based on health plan coverage policies, averting $50K+ worth of potential losses during one quarter alone.
- Represented the organization at periodic meetings with government insurance agencies to discuss reimbursement issues and collaborated closely with internal stakeholders on related policy updates.
- Advised executive leadership team on strategies aimed at increasing overall compliance with governmental regulations while minimizing financial risks associated with non-compliance levels.
- Reorganized the revenue cycle process and operations, resulting in a 17% increase in monthly collection efficiency.
- Assessed and identified opportunities to optimize reimbursement strategies for various payers; successfully recovered $500K+ of previously unbilled claims over three months.
- Consistently monitored trends related to denials, rejections, underpayments and other payment issues; proactively addressed discrepancies before they had an impact on the bottom line.
- Spearheaded several projects aimed at reducing financial leakage by uncovering any billing errors or misaligned coding that led to claim denials; saved nearly $200K annually due to improved accuracy rates across all departments within the organization leading up submission of claims.
- Demonstrated expertise in identifying fraudulent activities through detailed analysis of provider contracts & fee schedules as well as patient demographics information; flagged potential threats in time which resulted in savings of over $350K yearly from missed payments and incorrect reimbursements.
- Improved revenue integrity processes by 10%, ensuring accuracy of revenue data across multiple sources and timely reconciliation of accounts.
- Revised billing policies to better align with industry standards, resulting in an additional $50K in recovered funds within a three-month period.
- Meticulously researched discrepancies between patient records and billings for up to 200 claims per day; identified error patterns which led to a reduction in overall denied payment applications by 5%.
- Expedited the review process for high dollar value claims, enabling healthcare providers to receive payments faster while maintaining compliance with government regulations and contractual agreements.
- Coordinated closely with insurance companies, medical staff & IT personnel on various projects related to charge capture accuracy & coding optimization; reduced turnaround time on claim follow-ups by 30% or more each month.
- Thoroughly analyzed and reviewed data to identify revenue leakage issues, resulting in a reduction of $200k in unpaid claims.
- Presented comprehensive findings on billing errors and discrepancies to the management team with proposed solutions; successfully implemented strategies that increased revenue by 8% over six months.
- Collaborated with IT teams to develop automated processes for tracking patient demographics and financial information; reduced manual entry time by 50%.
- Documented evidence-based audit rules including detailed descriptions of coding practices, payment guidelines, policies & procedures; improved accuracy rate from 80% to 98%.
- Structured monthly reports summarizing charge capture levels for various services provided at multiple locations within the healthcare system; identified process gaps leading to a 10% increase in accurate coding compliance rates within 6 months.
- Evaluated healthcare claims and revenue data to identify errors, inconsistencies or discrepancies; detected $2million in billing inaccuracies by conducting detailed audits.
- Utilized various software tools such as Microsoft Excel and SQL to analyze financial documents for trends and patterns related to reimbursement processes; identified overpayment issues that resulted in a savings of $500,000 annually.
- Efficiently handled all inquiries from external stakeholders regarding the organization’s compliance with Medicare/Medicaid regulations; improved accuracy rate of denials from 15% to 95%.
- Monitored changes in government policies affecting healthcare provider reimbursements on an ongoing basis and provided updates about any new requirements to leadership team members within 24 hours each time there was a shift in policy landscape.
- Formulated appropriate corrective actions based on audit results while ensuring adherence with local, state & federal laws governing medical billing practices; increased payment accuracy rate by 10% compared to year-earlier figures without compromising quality standards at any point during the process.
3. Skills
The skillset employers require in an employee will likely vary, either slightly or significantly; skimming through their job adverts is the best way to determine what each is looking for. One organization may require an expert in coding and another may need someone with experience of auditing.
It is therefore important to tailor the skills section of your resume to each job you are applying for, as many employers use applicant tracking systems (ATS) these days which scan resumes for certain keywords before passing them on to a human.
Once listed here, it is also beneficial to elaborate further on some key skills in other areas such as the summary or experience sections; this will help demonstrate why you would be a great fit for the role.
Below is a list of common skills & terms:
- Coding and Billing
- Compliance Auditing
- Contract Negotiation
- Data Analysis
- Financial Reporting
- HIPAA Regulations
- ICD-10 Coding
- Medical Terminology
- Medicare/Medicaid Regulations
- Revenue Cycle Management
4. Education
Adding an education section on your resume will depend on how far along you are in your career. If you just graduated and have no work experience, it is important to include an education section below your resume objective. However, if you have significant work experience to showcase, omitting the education section altogether might be a better option.
If an education section is included, try to mention courses relevant to the revenue integrity analyst role you are applying for such as accounting or finance classes.
Bachelor’s Degree in Accounting
Educational Institution XYZ
Nov 2011
5. Certifications
Certifications are a great way to demonstrate your expertise in a particular field. They show that you have been tested and certified by an authoritative body, which can be highly beneficial when applying for jobs.
Including certifications on your resume is especially important if the job advert specifically mentions certain skills or qualifications. This will help prove to potential employers that you are qualified for the role and stand out from other applicants who may not possess such credentials.
Certified Revenue Integrity Analyst
American Association of Professional Coders
May 2017
6. Contact Info
Your name should be the first thing a reader sees when viewing your resume, so ensure its positioning is prominent. Your phone number should be written in the most commonly used format in your country/city/state, and your email address should be professional.
You can also choose to include a link to your LinkedIn profile, personal website, or other online platforms relevant to your industry.
Finally, name your resume file appropriately to help hiring managers; for Logan Morar, this would be Logan-Morar-resume.pdf or Logan-Morar-resume.docx.
7. Cover Letter
Writing a cover letter is an essential part of the job application process. It is a document that gives employers more information about you and why you’re a great fit for their role.
Cover letters are typically 2 to 4 paragraphs long and should provide additional details not mentioned in your resume. They can be used to demonstrate your personality, highlight key skills or explain any gaps in employment history.
Although cover letters aren’t always required, they offer many benefits that could help increase your chances of securing an interview.
Below is an example cover letter:
Dear Terrill,
I am writing to apply for the Revenue Integrity Analyst position at XYZ Company. I am a recent graduate of ABC University with a degree in Business Administration and a concentration in Accounting. I also have two years of experience working as an intern in XYZ Company’s accounting department. In my current role, I work closely with the revenue cycle team to ensure that all charges are accurately coded and billed. My experience and education make me uniquely qualified for this position, and I am confident that I can be an asset to your team.
As an analyst, it is important to be able to identify trends and problems quickly so that they can be addressed before they become bigger issues. My analytical skills are one of my strongest assets, and I have used them extensively in my current role. In addition, my ability to effectively communicate with people at all levels is another strength that would benefit me in this position.
I believe that my qualifications make me the ideal candidate for this job, and I look forward to discussing how I can contribute to your team’s success. Thank you for your time and consideration; please do not hesitate to contact me if you have any questions or need additional information about my qualifications.
Sincerely,
Logan
Revenue Integrity Analyst Resume Templates
 Gharial
Gharial Axolotl
Axolotl Jerboa
Jerboa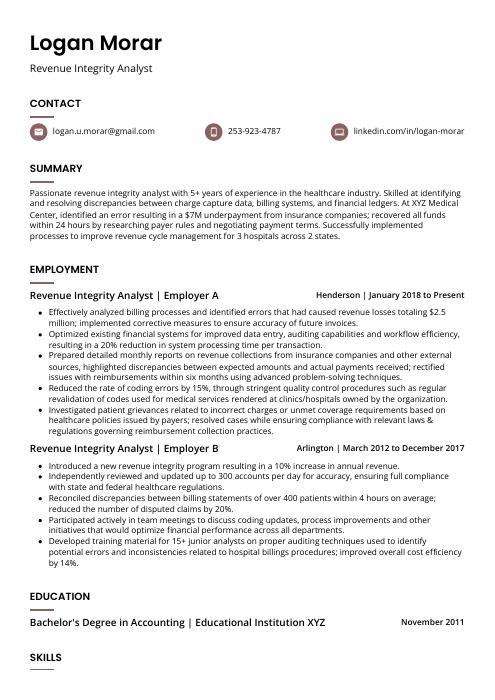 Fossa
Fossa Numbat
Numbat Kinkajou
Kinkajou Saola
Saola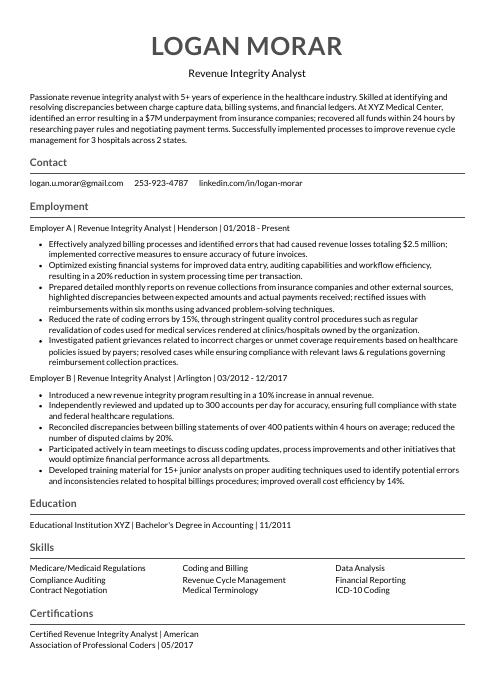 Indri
Indri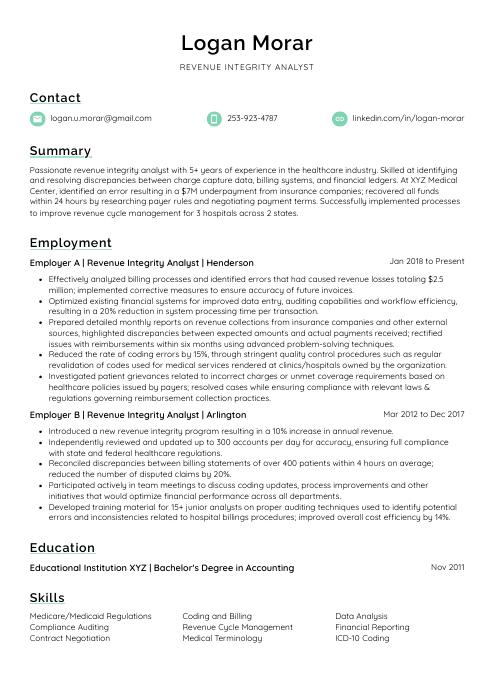 Lorikeet
Lorikeet Echidna
Echidna Dugong
Dugong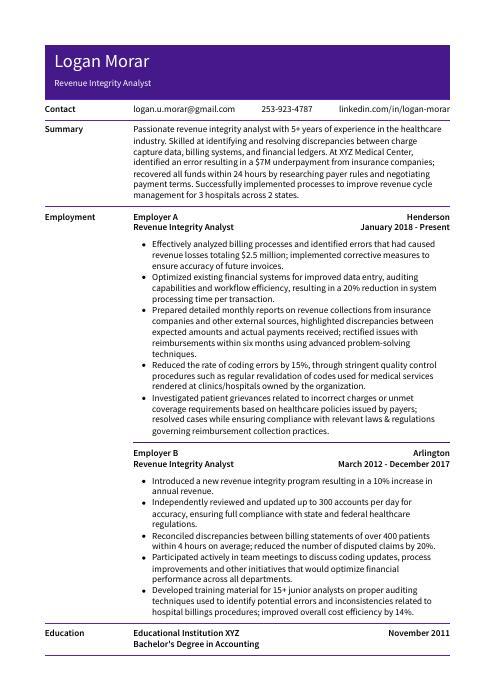 Pika
Pika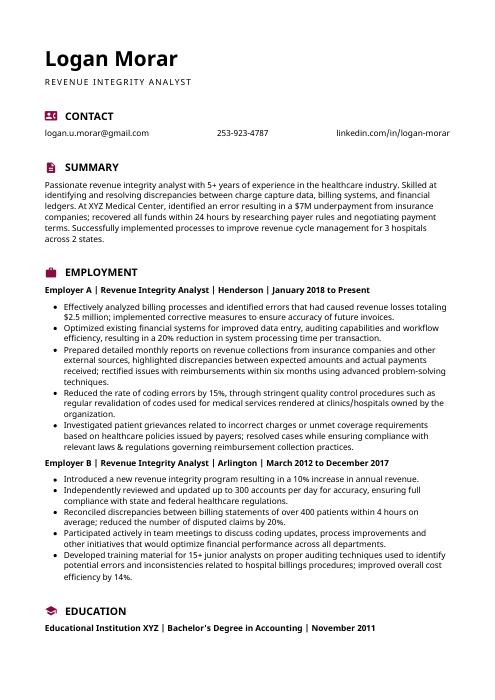 Hoopoe
Hoopoe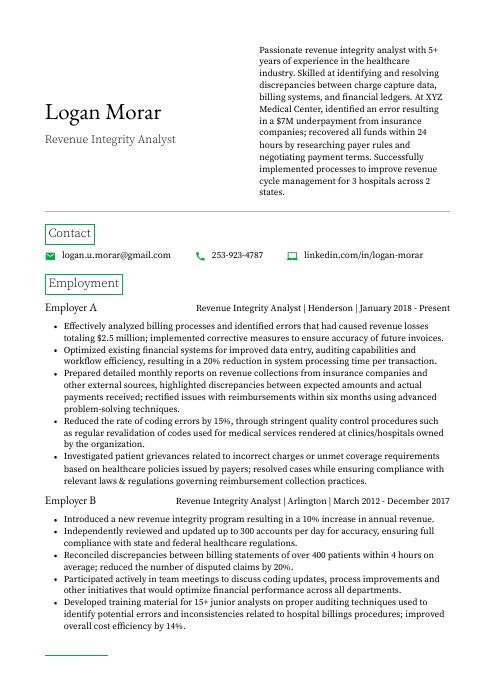 Quokka
Quokka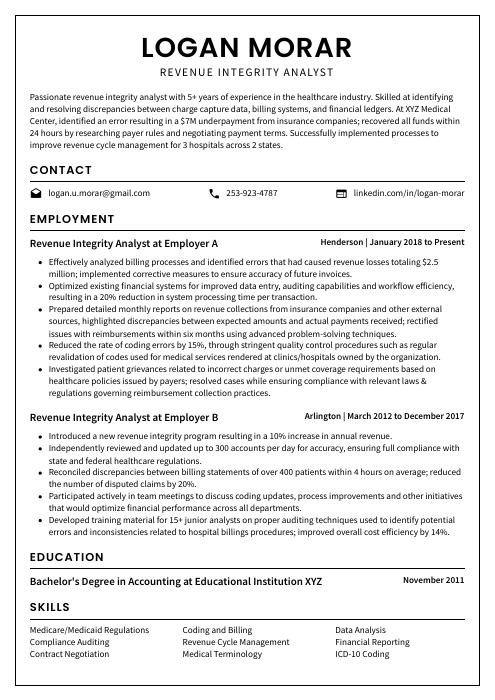 Cormorant
Cormorant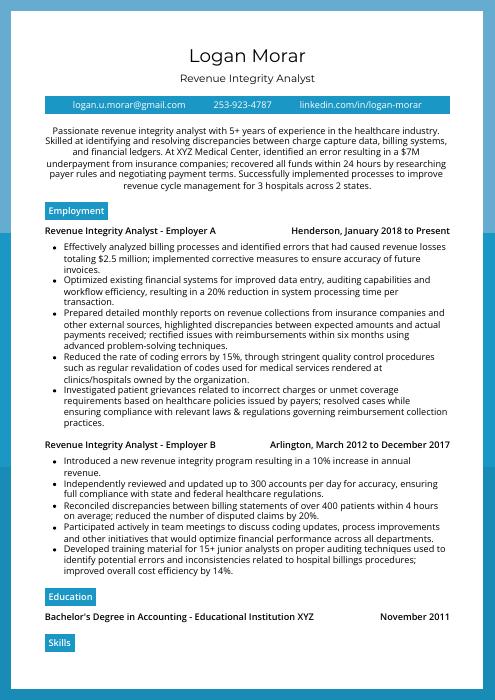 Rhea
Rhea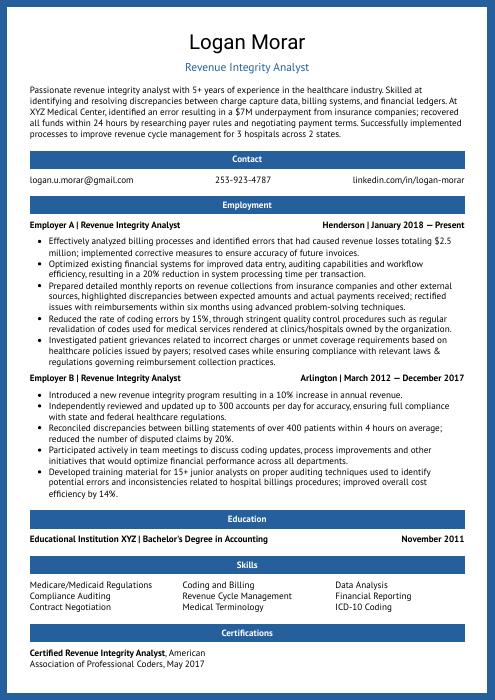 Ocelot
Ocelot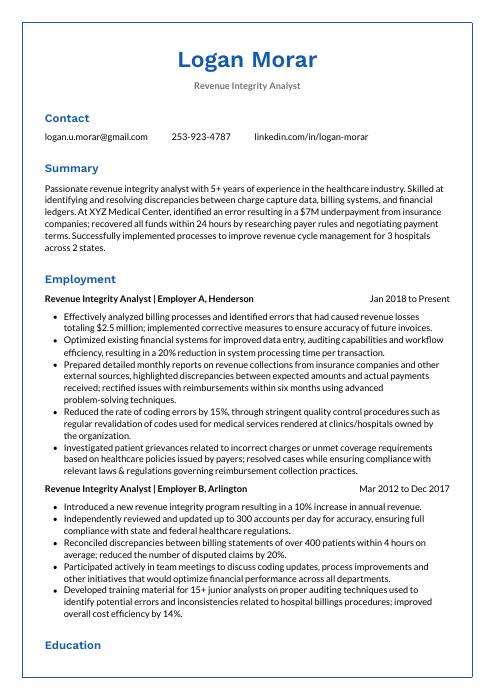 Markhor
Markhor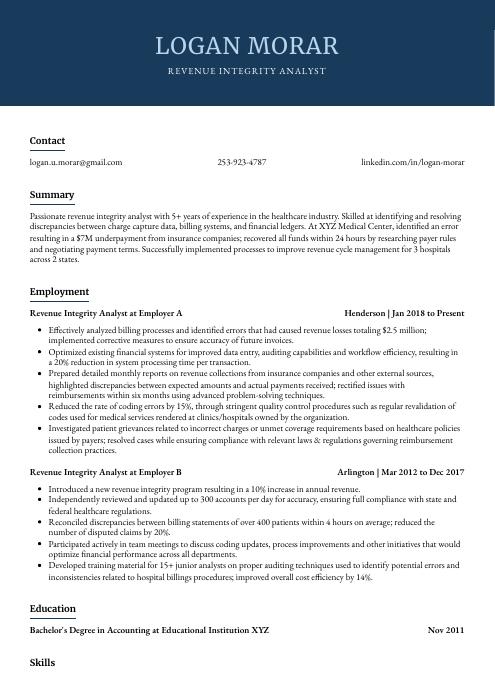 Bonobo
Bonobo Rezjumei
Rezjumei